Generic vs Brand Name Drugs: What the Label Really Tells You
 Dec, 1 2025
Dec, 1 2025
Generic Drug Cost Savings Calculator
How This Calculator Works
Based on FDA data, generic drugs typically cost 80-85% less than brand-name equivalents. This calculator shows your potential savings when switching to generics.
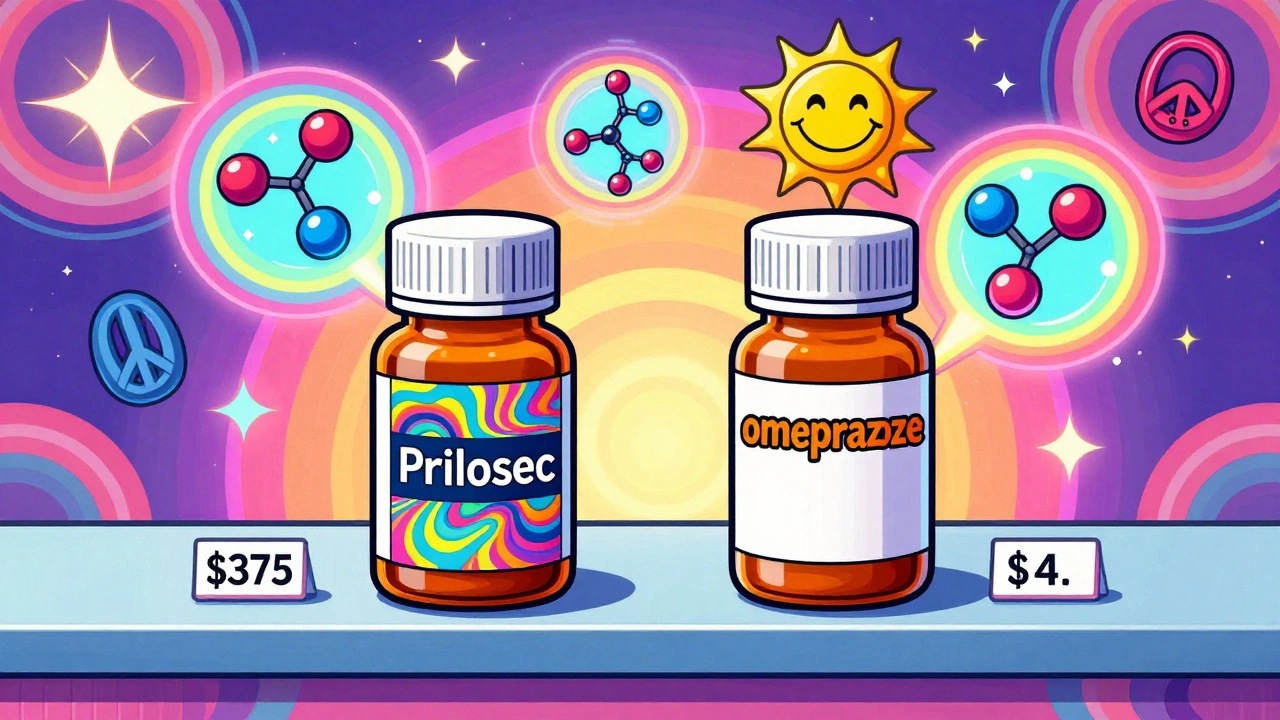
When you pick up a prescription, you might see two very different labels on the bottle. One says Prilosec, the other says omeprazole a proton pump inhibitor used to treat acid reflux and ulcers. One costs $375 a month. The other costs $4. You might wonder: is the cheaper one just as good? The answer isn’t just yes - it’s backed by science, regulation, and real-world use.
Same Active Ingredient, Different Look
Generic drugs and brand-name drugs contain the exact same active ingredient, in the same strength, and work the same way in your body. That’s not a guess. It’s a legal requirement enforced by the U.S. Food and Drug Administration (FDA). If a generic version of Lipitor (atorvastatin) is approved, it must deliver the same amount of atorvastatin into your bloodstream at the same rate as the brand-name version. The FDA calls this bioequivalence.To prove it, manufacturers run tests on 24 to 36 healthy volunteers. They measure how much of the drug enters your blood (Cmax) and how long it stays there (AUC). The generic must fall within 80% to 125% of the brand’s numbers. That’s tighter than the natural variation you’d see between two different batches of the same brand-name drug. As Dr. Ameet Nagpal from Northwestern Medicine put it, the 20% allowance isn’t a loophole - it’s a safety buffer built into the system.
So why do they look different? U.S. trademark laws require generic pills to look different from brand-name ones. That means different colors, shapes, sizes, or markings. A blue oval Lipitor becomes a white oval pill with "ATV 20" stamped on it. This isn’t about effectiveness - it’s about avoiding legal confusion. The active ingredient? Identical.
Labeling: What’s Changed, What’s Not
The FDA requires generic drug labels to match brand-name labels in every medically important way. That includes:- Indications (what the drug treats)
- Dosage instructions
- Warnings and contraindications
- Possible side effects
- Storage conditions
So if your brand-name drug says "avoid grapefruit juice," so does the generic. If it warns about liver damage, the generic carries the same warning. The only real difference? The name on the label. Brand-name drugs use proprietary names like "Crestor" or "Viagra." Generics use the chemical name: "rosuvastatin" or "sildenafil."
Some people get confused when they see their pill change color or shape. That’s not a sign the drug changed - it’s just a different manufacturer. Many generics are made by the same companies that make brand-name drugs. Teva, Sandoz, and Amneal - the top three generic makers - all produce both branded and generic products. The difference is in marketing, not manufacturing.
Cost: The Real Difference
This is where generics win by a landslide. In 2023, generic drugs accounted for 90% of all prescriptions filled in the U.S., but only 25% of total drug spending. That’s because they cost 80% to 85% less.Take atorvastatin. The brand-name Lipitor cost $375.22 per month in Q2 2023. The generic? $4.00 at Walmart. Omeprazole (Prilosec) went from $150 a month to under $10. Metformin (Glucophage) dropped from $120 to $4. These aren’t outliers. The FDA says 90% of generic drugs cost less than $10 per month.
The savings add up fast. From 2007 to 2016, generic drugs saved the U.S. healthcare system $1.67 trillion. In 2023 alone, they saved $313 billion. That’s money that keeps people on their meds instead of skipping doses because they can’t afford them. A Kaiser Permanente survey found that 78% of patients said cost savings from generics helped them fill prescriptions consistently.

Therapeutic Equivalence: Proven, Not Assumed
A 2021 study in JAMA Internal Medicine tracked over 2 million patients taking generic versus brand-name cardiovascular drugs. No difference in heart attacks, strokes, or deaths. A 2023 review in BMJ Open analyzed 47 clinical trials - again, no evidence that generics were less effective.Even patients notice. On Drugs.com, generic atorvastatin has a 6.6/10 rating from nearly 2,000 reviews. Lipitor? 6.3/10 from under 900. People report the same results, same side effects - just lower bills.
But there’s one exception: narrow therapeutic index (NTI) drugs. These are medications where even tiny changes in blood levels can cause harm. Warfarin (a blood thinner), levothyroxine (for thyroid), and phenytoin (for seizures) fall into this category. For these, doctors often monitor blood levels closely when switching between brands or generics. The FDA doesn’t say generics are unsafe - they say these drugs need extra care. Pharmacists will often stick with the same manufacturer if you’re on one of these.
What About Complex Drugs?
Not all drugs are easy to copy. Insulins, biologics, and drug-device combos like EpiPens are harder to replicate. That’s why only 28% of biologic prescriptions are filled with generics (called biosimilars). The FDA approved its first generic version of semaglutide (Ozempic) in September 2023 - a big step forward. But these drugs require more complex testing, which is why they’re slower to enter the market.The FDA’s 2024-2028 plan aims to speed up approval of complex generics. In 2022, they approved 79 complex generics - up 22% from the year before. That’s a sign things are moving in the right direction.

How to Know If a Generic Is Right for You
You don’t need to be a pharmacist to make the right choice. Here’s how:- Check the FDA’s Orange Book. It lists approved generics and their therapeutic equivalence ratings. Look for "A" ratings - that means they’re approved as interchangeable.
- Ask your pharmacist. They know which generics are available and whether your insurance prefers one over another.
- Don’t panic over color changes. If your pill looks different, it’s likely a different manufacturer - not a different drug.
- For NTI drugs, ask your doctor if you need blood tests after switching.
- Use the FDA’s Generic Drug Program Dashboard to see if a new generic is coming soon.
Most doctors are comfortable prescribing generics. The American Medical Association found 94% of physicians feel confident doing so. And in 49 states, pharmacists can automatically switch you to a generic unless your doctor writes "Dispense as Written." That’s not a loophole - it’s a system designed to save money without sacrificing care.
Why This Matters for You
Choosing a generic isn’t about cutting corners. It’s about using a system that’s been tested, regulated, and proven over decades. The FDA doesn’t approve generics because they’re cheap - they approve them because they work just as well.If you’re on a chronic medication - blood pressure, cholesterol, diabetes, thyroid - switching to a generic could save you hundreds, even thousands, a year. That’s money for groceries, rent, or filling another prescription. And you won’t sacrifice safety or effectiveness.
The real question isn’t whether generics work. It’s why anyone still pays full price when a proven, cheaper alternative exists.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for quality, safety, and effectiveness as brand-name drugs. They must contain the same active ingredient, in the same strength, and work the same way in your body. All generics are reviewed and approved before they reach the market, and the FDA continues to monitor them through its adverse event reporting system.
Why do generic pills look different?
U.S. trademark laws require generic drugs to look different from brand-name versions to avoid confusion. That means different colors, shapes, sizes, or markings. These changes affect only the appearance - not the active ingredient, dosage, or how the drug works in your body.
Can I switch from a brand-name drug to a generic without problems?
For most drugs, yes. Over 90% of prescriptions are for drugs where switching poses no risk. For drugs with a narrow therapeutic index - like warfarin, levothyroxine, or phenytoin - your doctor may want to monitor your blood levels after switching. But even in those cases, the generic is still safe - it just requires a little extra attention.
Do generics take longer to work?
No. Bioequivalence testing ensures that generics enter your bloodstream at the same rate and to the same extent as the brand-name version. If the brand works in 30 minutes, so does the generic. Any delay you notice is likely due to individual differences in digestion or metabolism - not the drug itself.
Why are some generics more expensive than others?
Price differences between generic manufacturers happen due to supply, competition, and distribution. One company might have a better deal with a wholesaler, or there might be a temporary shortage. If one generic costs more than another, ask your pharmacist if a cheaper option is available. The active ingredient is still the same.
Is it true that generics are made in worse factories?
No. The FDA inspects all manufacturing facilities - whether they make brand-name or generic drugs - using the same standards. Many brand-name companies also make generic versions in the same factories. The difference is in branding, not quality control.
What’s Next?
The future of generics is growing. With over $268 billion in brand-name drug sales set to face generic competition between 2023 and 2028, more affordable options are coming. The FDA is speeding up reviews for complex generics, and new biosimilars for biologics are entering the market. The goal isn’t just to cut costs - it’s to make sure everyone can afford the medicines they need.If you’re on a long-term medication, ask your doctor or pharmacist if a generic is right for you. You might be surprised how much you can save - without giving up anything that matters.
Jaswinder Singh
December 2, 2025 AT 07:32Bro this is why people die from not taking meds. I saw my cousin skip his blood pressure pills because he thought the generic was ‘fake’ - ended up in the ER. The science’s solid. Stop overthinking and save your damn money.
Bee Floyd
December 2, 2025 AT 23:17Been taking generic atorvastatin for 5 years. Same results, same side effects (hello, muscle cramps), half the cost. My pharmacist even told me the same company makes both. Weird how marketing makes people think color = quality.
Eric Vlach
December 3, 2025 AT 17:23Generics are the unsung heroes of healthcare. Nobody throws a parade for the $4 pill that keeps grandma off the ventilator. But they should. The FDA doesn't cut corners and neither should we
Souvik Datta
December 4, 2025 AT 21:58As someone who’s seen patients choose between insulin and groceries, I can tell you this: generics aren’t just convenient - they’re life-saving. The real tragedy isn’t the pill color. It’s that we still treat medication like a luxury.
Priyam Tomar
December 6, 2025 AT 21:36Oh please. I’ve had generics that made me dizzy. The FDA’s ‘80-125% bioequivalence’ is a joke. That’s a 45% swing! You think that’s safe for someone on seizure meds? You’re lucky if you don’t end up in a coma.
Jack Arscott
December 8, 2025 AT 17:32✅ Generic = same active ingredient
✅ Same FDA standards
✅ 85% cheaper
❌ No magic dust
❌ No hidden toxins
💯 Just science and savings
Irving Steinberg
December 9, 2025 AT 00:25Why are people still buying brand name? Like… what are you even paying for? The box? The logo? The feeling that you’re somehow better because your pill is blue? 🤡
Lydia Zhang
December 10, 2025 AT 17:59My pharmacy switched my generic last month. Pill looks different. Still works. Done.
Kay Lam
December 11, 2025 AT 04:52I used to think generics were inferior until I started researching the FDA’s bioequivalence standards and realized that even the brand-name drugs have natural variability between batches - and yet we don’t panic when our Lipitor batch from last month feels different. The system works. It’s not perfect but it’s rigorously tested and the data shows no clinically meaningful difference for the vast majority of medications. People get scared because they don’t understand pharmacokinetics or how the body metabolizes drugs, but the science is clear and the savings are enormous - we’re talking billions saved annually, and that means people aren’t skipping doses because they can’t afford their meds. That’s not just economics - that’s public health.
Adrian Barnes
December 12, 2025 AT 04:08While the FDA’s regulatory framework appears robust on paper, the systemic erosion of manufacturing oversight in recent years - particularly with offshore facilities - renders the notion of ‘equivalence’ a statistical illusion. The 80-125% bioequivalence window is not a safety buffer - it is a regulatory abdication. When you compound this with the fact that 78% of generic manufacturing occurs in India and China, where inspections are infrequent and corruption is endemic, the assertion that generics are ‘just as safe’ becomes not just misleading - it is dangerously irresponsible. The data you cite ignores confounding variables: patient adherence, pharmacogenomic variability, and the psychological placebo effect of brand association - all of which influence clinical outcomes. To recommend generics as universally equivalent is to ignore the very nature of human physiology.
patrick sui
December 13, 2025 AT 11:02Interesting how the FDA’s 80-125% range is often misunderstood. It’s not a ‘loophole’ - it’s a statistically validated tolerance band accounting for inter-individual pharmacokinetic variance. In fact, intra-brand variability between two batches of Lipitor can exceed 15%. The real issue isn’t the generic - it’s the lack of patient education. We’re teaching people to equate price with quality, which is a cognitive bias rooted in behavioral economics. Also, fun fact: 40% of ‘brand-name’ drugs are manufactured by the same facilities as generics - just different packaging and marketing spend. The real villain here isn’t the pill - it’s the pharmaceutical marketing machine.
Declan O Reilly
December 14, 2025 AT 16:14Imagine if cars worked like this. You buy a Toyota Camry, then they give you a ‘generic Camry’ that’s identical in engine, safety rating, and mileage - but painted gray and costs $5k. You’d be like ‘why did I pay $25k before?!’ But for pills? We’re still scared of the gray one. We’ve been conditioned to think ‘expensive = better’ - even when the data screams otherwise. The system is rigged to sell you a brand, not a cure.
Conor Forde
December 16, 2025 AT 10:10Y’all are so naive. The FDA is a corporate puppet. I got a generic version of my thyroid med and I swear to god I felt like I was drowning in slow motion for three weeks. My doctor said ‘it’s the same’ - yeah right. The pill had a different filler. Probably talc. Or asbestos. Or whatever they pump into Chinese factories. You think the FDA inspects every batch? LOL. I’m switching back to the $150 version. My life’s worth more than $4.