Bioequivalence for Inhalers, Patches, and Injections: How Generic Drugs Match the Real Thing
 Dec, 18 2025
Dec, 18 2025
When you pick up a generic inhaler, patch, or injection, you expect it to work just like the brand-name version. But here’s the truth: bioequivalence for these complex delivery systems isn’t just about matching the amount of drug in the bottle. It’s about making sure the drug gets to the right place in your body at the right speed - and that’s far harder than it sounds.
Why Bioequivalence Isn’t the Same for Inhalers, Patches, and Injections
For a pill, bioequivalence is straightforward. You swallow it, the drug enters your bloodstream, and you measure how much shows up in your blood over time - the Cmax (peak concentration) and AUC (total exposure). If the generic’s numbers fall within 80-125% of the brand, it’s considered equivalent. But that doesn’t work for inhalers, patches, or injections with complex formulations. Why? Because the drug isn’t meant to circulate widely. For an asthma inhaler, the drug needs to land in your lungs. For a nicotine patch, it slowly seeps through your skin. For a liposomal injection, it’s designed to hide in tiny fat bubbles until it reaches a tumor. If the particle size, delivery mechanism, or release rate is off by a fraction, the drug might not work - or worse, it could cause side effects. The FDA, EMA, and other regulators realized this decades ago. By 2011, they started publishing special guidance for each delivery system. The rules got stricter. The testing got more expensive. And the approval rates dropped.Inhalers: It’s Not Just the Drug - It’s the Plume
A generic albuterol inhaler might contain the exact same amount of medicine as the brand. But if the aerosol plume is 2°C warmer, or if 10% more particles are too big to reach the lungs, the FDA will reject it. Why? Because those particles get stuck in your throat or mouth instead of your airways. To prove bioequivalence, manufacturers must pass two tests:- In vitro: Particle size must be 90% between 1-5 micrometers. The device must deliver exactly the same dose per puff - within 75-125% of the label. The plume shape, speed, and temperature must match the original.
- In vivo: For systemic effects (like beta-agonists), they measure blood levels. For inhaled steroids, they measure lung function - like FEV1 (how much air you can force out in one second). If your lung function doesn’t improve the same way, it’s not equivalent.
Transdermal Patches: Slow and Steady Wins the Race
Patches are designed to release drug slowly over hours or days. That means Cmax isn’t a reliable measure. A generic patch might hit a higher peak early, then drop too fast - leaving you with no pain relief by nightfall. The FDA requires:- In vitro release: The patch must release the same amount of drug at every time point - within 10% of the brand. This is tested using Franz diffusion cells, which mimic skin.
- Adhesion and skin contact: If the patch peels off early or doesn’t stick well, you won’t get the full dose. Manufacturers must prove it stays on during normal movement, sweat, and bathing.
- AUC is king: Since the drug enters slowly, the total exposure (AUC) must fall within 80-125%. Cmax can vary more, as long as the overall effect is the same.

Injectables: When the Bottle Isn’t Enough
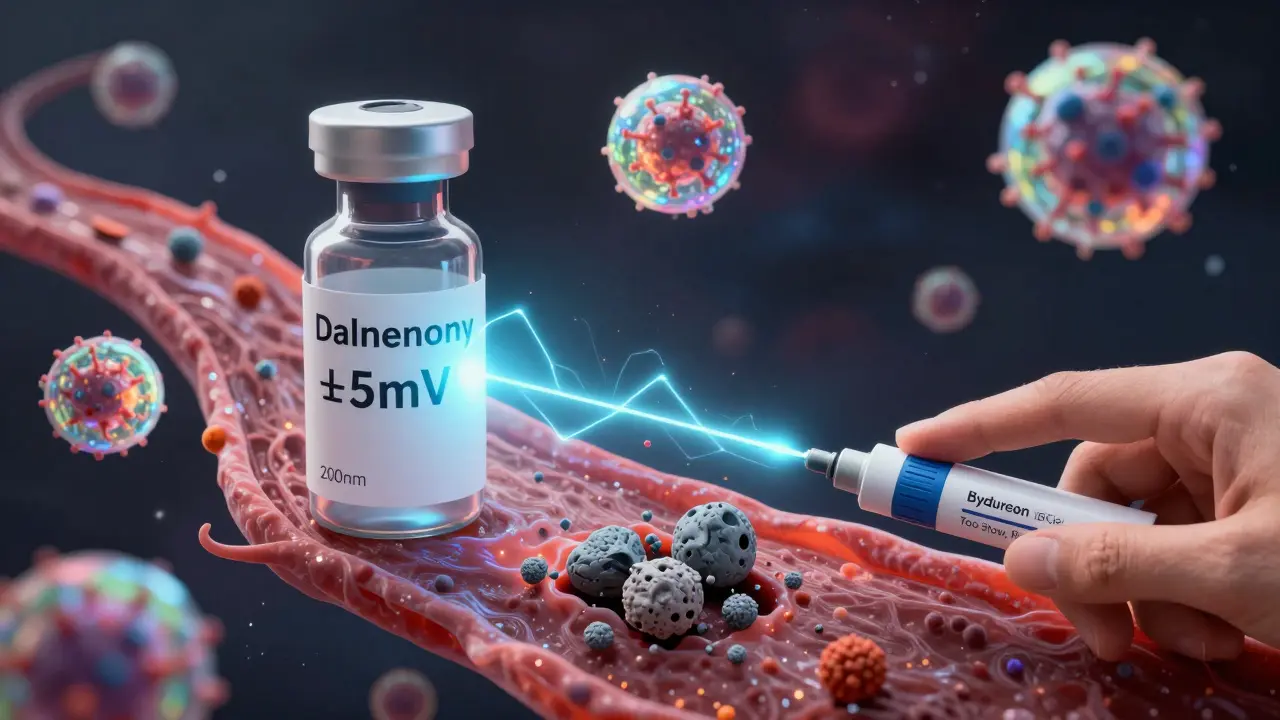
Not all injections are the same. A simple saline solution? Easy. A nanoparticle-loaded cancer drug? Not even close. For complex injectables - like liposomal doxorubicin or enoxaparin (Lovenox) - regulators demand proof that the physical structure is identical:- Particle size: Must be within 10% of the brand. A 200-nanometer particle vs. a 220-nanometer particle can change how the drug is absorbed.
- Zeta potential: This measures surface charge. A difference of more than 5mV can cause the particles to clump or break down too fast.
- In vitro release: The drug must leak out at the same rate over time - tested in simulated body fluids.
The Cost of Getting It Right
Developing a generic pill? $5-10 million. Two years. Developing a generic inhaler? $25-40 million. Four years. Why the jump? You need specialized labs:- Cascade impactors ($150K-$300K) to measure particle size in inhalers
- Franz cells ($50K-$100K) to test patch release
- Nanoparticle analyzers ($200K+) for injectables
Who’s Winning and Who’s Losing
Teva, Mylan, and Sandoz dominate the space. Together, they have 31 approved complex generics. Teva’s generic ProAir RespiClick succeeded because they used scintigraphy imaging - a technique that literally shows where the drug lands in the lungs. That kind of proof convinced regulators. But small companies? Most can’t afford it. The FDA has helped 42 small businesses since 2018, but the barrier remains high. That’s why, even though complex delivery systems make up 30% of prescriptions, they account for only 15% of the generic market by value. The high cost keeps competition low - and prices high.The Future: PBPK Models and Patient-Centered Testing
The next wave of bioequivalence isn’t just about labs. It’s about real people. Regulators are starting to accept physiologically-based pharmacokinetic (PBPK) modeling - computer simulations that predict how a drug behaves in different body types. In 2022, 65% of complex generic submissions included PBPK data, up from 22% in 2018. The EMA now requires patient training materials to be part of the equivalence package for inhalers. Because if you don’t inhale the way the device was designed for, the drug won’t work - even if the generic matches the brand perfectly in the lab. And there’s a quiet danger: "biocreep." When multiple generics are made over time, each one slightly different, those tiny changes can add up. A 2022 study warned that after three or four generations of generics, the cumulative effect could reduce effectiveness - without anyone noticing until patients start having worse outcomes.What This Means for You
If you’re prescribed a generic inhaler, patch, or injection, you can trust it - if it’s been approved by the FDA or EMA. The process is brutal, expensive, and meticulous. Regulators don’t cut corners on these. But if your insurance switches your generic without telling you, ask. Not all generics are created equal. And for complex delivery systems, the difference between "equivalent" and "effective" can be measured in micrometers and millivolts. The goal isn’t just cheaper drugs. It’s drugs that work - exactly as they should.What does bioequivalence mean for inhalers?
For inhalers, bioequivalence means the generic must deliver the same amount of drug in the same particle size range (1-5 micrometers), with identical plume shape, speed, and temperature. It must also produce the same clinical effect - like improved lung function - when tested in patients. Just matching drug concentration in the blood isn’t enough.
Why are generic patches harder to approve than pills?
Patches release drug slowly through the skin, so peak blood levels (Cmax) aren’t reliable. Regulators require proof that the drug releases at the same rate over time (in vitro), sticks to skin the same way, and delivers the same total amount (AUC). Even a 10% difference in release rate can mean the difference between relief and breakthrough pain.
Can a generic injection be approved without testing in humans?
Rarely. For complex injectables like liposomes or nanoparticles, regulators require proof that the physical structure - particle size, charge, and release profile - matches the brand. Human pharmacokinetic studies are almost always required because lab tests alone can’t predict how the body will react.
Why are so few generic inhalers on the market?
Because the requirements are extreme. Manufacturers must match particle size, dose delivery, plume geometry, and clinical lung response. Development costs average $32 million and take 4 years. Many companies can’t afford it - and even then, 62% of applications fail. Only a handful of companies have the expertise and resources to succeed.
Are generic complex delivery systems safe?
Yes - if they’re approved by the FDA or EMA. These agencies require more testing for complex generics than for any other drug type. Every step - from particle size to patient inhalation technique - is scrutinized. The rejection of generics like Advair Diskus and Bydureon BCise shows regulators won’t approve anything that doesn’t match the original in every meaningful way.
Nina Stacey
December 19, 2025 AT 16:56Man I just got prescribed a generic inhaler last month and was kinda nervous but after using it for a few weeks I can barely tell the difference
My lungs feel the same and I’m not coughing more than usual
Maybe the system works better than people think
Dominic Suyo
December 21, 2025 AT 05:24Oh please. The FDA’s ‘approval’ is just corporate theater wrapped in a lab coat
They let through generics with 3% variance in zeta potential and call it ‘equivalent’
Meanwhile patients are getting subtherapeutic doses because some bean counter cut corners on nanoparticle characterization
It’s not bioequivalence - it’s biocreep in slow motion and nobody’s paying attention until someone codes
Marsha Jentzsch
December 22, 2025 AT 09:07Okay but have you ever actually read the patient inserts for these generics??
They’re all different!!
And the instructions? Sometimes they say ‘inhale deeply’ and sometimes they say ‘breathe slowly’
That’s not an accident - that’s the manufacturers trying to cover their butts because they know their product doesn’t match the original
And don’t even get me started on the patches peeling off in the shower - I’ve had three different generics and none of them stayed on like the brand
It’s a scam
Janelle Moore
December 23, 2025 AT 14:24They’re hiding something
Big Pharma owns the FDA
They want you to think generics are safe but they’re just letting bad ones through so you keep buying more
Remember the Vioxx scandal? Same playbook
They’ll kill you slowly with a cheaper patch and then charge you $800 for the brand again when you get sick
They’re not here to help you
They’re here to profit
Danielle Stewart
December 25, 2025 AT 07:05Really appreciate this breakdown - I work in pharmacy and see this every day
It’s not just about the drug, it’s about the whole delivery system
And honestly? Most patients don’t realize how much technique matters with inhalers
One of my patients used her generic inhaler wrong for months because the instructions were printed smaller and she didn’t notice
That’s why the EMA now requires training materials - it’s not just science, it’s education
mary lizardo
December 26, 2025 AT 11:33The notion that bioequivalence can be meaningfully established for complex delivery systems without in vivo human trials is scientifically indefensible.
Regulatory agencies have capitulated to cost-efficiency imperatives at the expense of clinical fidelity.
The 80–125% AUC range is a statistical fiction when applied to transdermal or liposomal pharmacokinetics.
One must ask: if the drug’s behavior cannot be fully modeled in vitro, why is human testing not mandatory for all cases?
It is not merely a matter of economics - it is an ethical failure.
Kelly Mulder
December 26, 2025 AT 23:47So you’re telling me a 3% difference in particle size can make a patient bleed out?
And we’re letting this happen because it’s cheaper?
Wow.
Just wow.
Big Pharma wins again.
Meanwhile, my cousin’s dad died from a generic Lovenox he got at Walmart.
They didn’t even tell him it was generic.
They just swapped it.
And now he’s in the ground.
And the FDA? They’re still approving these things.
Unbelievable.
Tim Goodfellow
December 28, 2025 AT 14:59Whoa - I had no idea inhalers were this complicated
It’s not just the drug - it’s the plume, the temp, the particle size, the lung function
It’s like trying to replicate a symphony by just matching the sheet music
But missing the conductor, the instruments, the acoustics
And somehow we still think it’s the same song?
That’s wild
And the fact that Teva used scintigraphy to prove theirs works? That’s next level
Science porn right there
Elaine Douglass
December 30, 2025 AT 02:30I’ve been on a generic patch for years and it’s been fine for me
But I get why some people have issues
Maybe it’s just not for everyone
And if your insurance switches it without telling you, that’s rough
Just talk to your pharmacist - they’ll help you figure it out
Don’t panic, but don’t ignore it either
Small changes matter
Takeysha Turnquest
December 30, 2025 AT 08:00We think drugs are magic pills
But they’re not
They’re messages
Delivered by machines we don’t understand
And when the machine changes
The message gets lost
And we wonder why we’re still sick
It’s not the drug
It’s the delivery
It’s the silence between the words
Alex Curran
December 30, 2025 AT 15:12Just wanted to add - the cascade impactor isn’t just expensive, it’s finicky
One lab’s calibration can differ from another’s by 5% just from humidity
And if the lab tech is tired or rushed? You get bad data
That’s why IVIVC models are so hard to build
It’s not just science - it’s art
And only a few labs in the world can do it right
That’s why only 35% of companies succeed
It’s not lack of will - it’s lack of capability
Edington Renwick
December 31, 2025 AT 00:39Let me get this straight
You’re telling me a generic inhaler was rejected because the plume was 2°C warmer?
And that’s why it failed?
And yet, my cousin’s cousin’s neighbor got a generic patch that melted in her purse and didn’t work for three days?
But that’s fine?
Why does the FDA care about temperature but not about patches falling off in the shower?
Who decided this was a priority?
And who’s paying for it?
Someone’s getting rich off this mess
Allison Pannabekcer
December 31, 2025 AT 11:52This is such an important topic and I’m glad someone took the time to explain it
It’s easy to assume generics are just cheaper versions
But for inhalers and patches? They’re like trying to copy a fingerprint
Even the tiniest difference changes everything
And I think what’s missing from this conversation is the patient’s voice
Who’s listening to the people who use these daily?
Maybe the next step isn’t just better labs - it’s better communication
Patients deserve to know what’s in their medicine - and how it’s really made
Aboobakar Muhammedali
January 1, 2026 AT 20:21I work in a clinic in Mumbai and we use a lot of generic inhalers
Most patients can’t afford the brand
So we test them carefully - lung function, symptom logs, rescue inhaler use
And honestly? Most generics work fine
But we watch for the ones that don’t - and we switch back fast
It’s not perfect
But in places like this, it’s the only way
Regulators in the US have luxury of time and money
Here? We make do
But we don’t ignore the signs