PCSK9 Inhibitors vs Statins: Side Effects and Outcomes Compared
 Jan, 11 2026
Jan, 11 2026
LDL Reduction Calculator
How Much Can You Lower Your LDL?
Enter your current LDL level to see expected reduction with statins or PCSK9 inhibitors. This calculator is based on clinical trial data from the article.
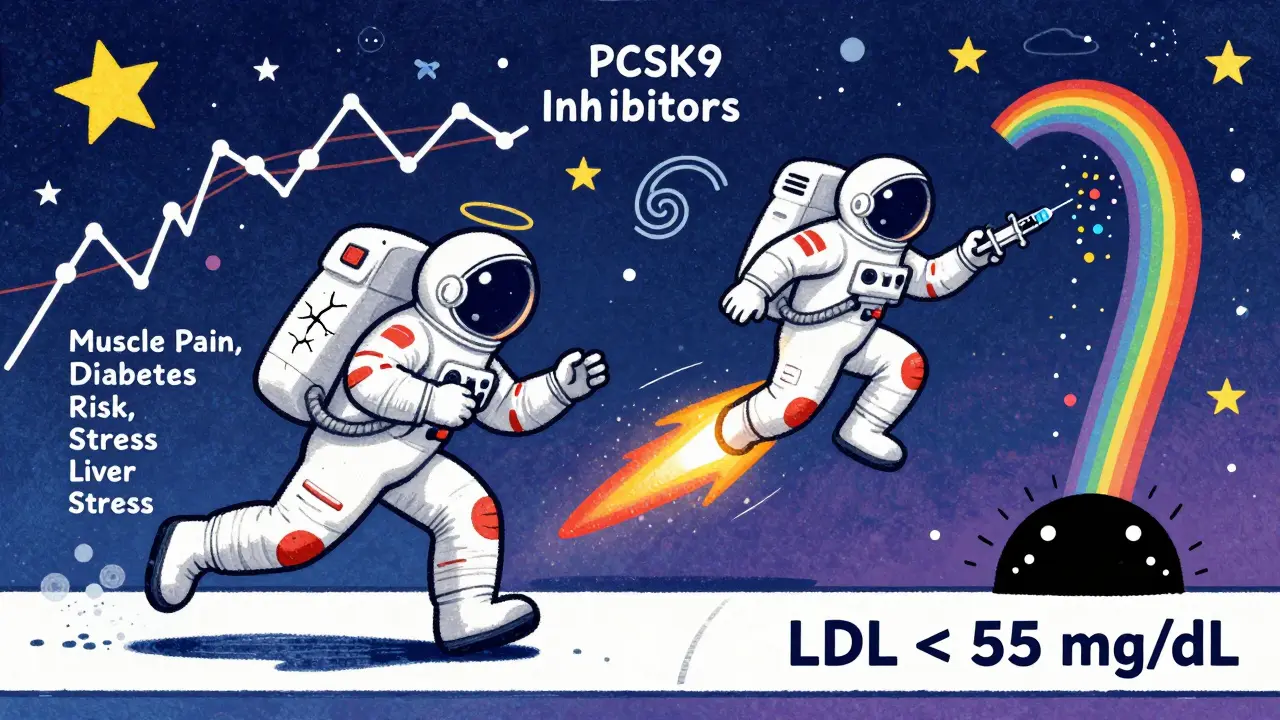
When it comes to lowering cholesterol, two main types of drugs dominate the conversation: statins and PCSK9 inhibitors. Both work to reduce LDL (bad) cholesterol, but they do it in completely different ways-and with very different trade-offs. If you’ve been told you need to lower your cholesterol, you’ve probably heard about statins. But if you’ve tried them and still have high numbers-or if you got muscle pain, fatigue, or brain fog-you might be wondering what else is out there. PCSK9 inhibitors are that something else. They’re not new, but they’re becoming more common for people who can’t get their LDL under control with statins alone.
How Statins Work (and Why They’re Still First-Line)
Statins have been around since the late 1980s. They block an enzyme in your liver called HMG-CoA reductase, which is responsible for making cholesterol. Less cholesterol production means your liver pulls more LDL out of your bloodstream to use as raw material. That’s how LDL levels drop-typically by 30% to 50%, depending on the dose and the specific statin. They’re cheap. Generic atorvastatin or rosuvastatin costs as little as $4 to $10 a month. They’re taken once a day, orally. Millions of people take them. They’ve been studied in over 100 large clinical trials spanning more than 30 years. The data is overwhelming: statins reduce heart attacks, strokes, and death in people with heart disease or high risk for it. But they’re not perfect. About 5% to 10% of people experience muscle pain, weakness, or cramps-sometimes severe enough to stop taking them. That’s called statin-associated muscle symptoms (SAMS). A 2023 study in Mayo Clinic Proceedings found that up to 29% of patients report muscle issues, though not all are directly caused by the drug. Other side effects include elevated liver enzymes (rarely dangerous), digestive upset, and reports of memory fog or confusion, though large studies haven’t confirmed a strong link. One surprising risk: statins slightly increase the chance of hemorrhagic stroke (bleeding in the brain) in certain people, especially those with high blood pressure or a history of stroke. UCLA research in 2023 showed a 22% higher risk compared to placebo. That’s not a reason to avoid statins for most people-but it’s something your doctor should weigh if you’re at risk.How PCSK9 Inhibitors Work (and Why They’re Different)
PCSK9 inhibitors are a newer class of drugs. They’re not pills. They’re injections you give yourself under the skin, either every two weeks or once a month. Two brands are approved in the U.S.: alirocumab (Praluent) and evolocumab (Repatha). A third, inclisiran (Leqvio), is a twice-yearly shot that works differently but targets the same pathway. These drugs block a protein called PCSK9, which normally tells liver cells to destroy LDL receptors. When PCSK9 is blocked, more receptors stay on the liver’s surface-and those receptors grab LDL out of your blood. The result? LDL drops by 50% to 61%, often more than even the highest-dose statins. The biggest advantage? Almost no muscle pain. In clinical trials, patients switching from statins to PCSK9 inhibitors reported significant relief from muscle symptoms. A 2024 review in Frontiers in Cardiovascular Medicine found that 79% of users praised PCSK9 inhibitors for avoiding the muscle side effects that plagued them on statins. They also don’t interact with liver enzymes like statins do. That means fewer drug interactions and less risk of liver toxicity. And unlike statins, they don’t raise the risk of hemorrhagic stroke. In fact, across 36 randomized trials, no increased risk was found.Side Effects: What You’ll Actually Experience
Statins and PCSK9 inhibitors have very different side effect profiles. Statins:- Muscle pain or weakness (5-10% of users)
- Digestive issues (nausea, constipation, diarrhea)
- Increased blood sugar (small risk of developing type 2 diabetes)
- Memory complaints (rare, and not consistently proven)
- Minor liver enzyme elevations (usually harmless)
- Slight increase in hemorrhagic stroke risk in high-risk groups
- Injection site reactions (redness, itching, bruising-reported by 15-20% of users)
- Headache or flu-like symptoms (rare)
- Neurocognitive effects (no proven link, unlike statins)
- No muscle pain, no liver toxicity, no increased diabetes risk
Effectiveness: Which Lowers LDL More?
Let’s talk numbers. If your LDL is 160 mg/dL: - A high-dose statin might bring it down to 80-110 mg/dL (30-50% reduction).- A PCSK9 inhibitor alone might bring it to 60-80 mg/dL (50-61% reduction).
- Combining both? You could hit 40-50 mg/dL (up to 75% reduction). That’s huge for people with familial hypercholesterolemia or advanced heart disease. The American Heart Association recommends LDL under 55 mg/dL for very high-risk patients. Most statins can’t get you there alone. PCSK9 inhibitors can. The FOURIER and ODYSSEY trials showed that adding evolocumab or alirocumab to statins reduced heart attacks and strokes by about 20-27% over two years in people who already had heart disease. That’s not just cholesterol lowering-it’s life-saving.
Cost and Accessibility: The Real-World Hurdle
Here’s the catch: PCSK9 inhibitors cost a lot. Generic statins: $4-$10/month.PCSK9 inhibitors: $5,000-$14,000/year before insurance. Most insurers won’t cover them unless you’ve tried and failed on at least two statins, or you have documented statin intolerance. Even then, you might need prior authorization, which can take weeks. A 2024 study in the American Journal of Managed Care found 87% of U.S. insurers require this step. But things are changing. Drugmakers now offer copay cards that reduce out-of-pocket costs to $0-$300/month for eligible patients. Some Medicare Advantage plans cover them with lower copays. And new competitors like inclisiran (Leqvio), given only twice a year, may ease the burden of frequent injections. Still, cost remains a barrier. Many patients who could benefit never start because they can’t afford it-or can’t get approval.

Who Gets Which Drug?
It’s not one-size-fits-all. Here’s how doctors typically decide:- Statins first: For most people with high cholesterol, especially those with diabetes, high blood pressure, or moderate heart disease risk. They’re proven, cheap, and easy.
- PCSK9 inhibitors: For patients with:
- Familial hypercholesterolemia (genetic high cholesterol)
- Heart disease or stroke with LDL still above 70 mg/dL on max statin dose
- Statin intolerance (muscle pain, liver issues, or other side effects)
- LDL above 100 mg/dL with very high-risk features (like multiple heart events)
- Combination therapy: For very high-risk patients who need LDL below 55 mg/dL. Many cardiologists now add a PCSK9 inhibitor to a high-intensity statin if the target isn’t met.
What About Other Options?
Statins and PCSK9 inhibitors aren’t the only tools. Ezetimibe (Zetia) lowers LDL by about 15-20% and is often added to statins. Bempedoic acid (Nexletol) is an oral pill that works like a statin but avoids muscle side effects-it’s good for people who can’t tolerate statins. Inclisiran (Leqvio) is a PCSK9-targeting shot given only twice a year, which is easier for people who dread injections. But none of these match the LDL-lowering power of PCSK9 inhibitors. And none have the same long-term safety data as statins.What’s Next?
The future of cholesterol treatment is moving toward more targeted, less frequent, and more tolerable options. Merck is testing an oral PCSK9 inhibitor (MK-0616) in Phase II trials. Early results show it lowers LDL by 60%-with no injections. If approved, it could change everything. Gene-silencing therapies like inclisiran are already here. They work by turning off the PCSK9 gene in the liver, so your body makes less of the protein. One shot lasts six months. That’s a game-changer for adherence. The bottom line? Statins are still the foundation. But for people who can’t tolerate them-or who need deeper LDL reduction-PCSK9 inhibitors are a powerful, safer alternative.Can PCSK9 inhibitors replace statins completely?
Not for most people. Statins are still the first choice because they’re proven, affordable, and reduce overall mortality. PCSK9 inhibitors are used when statins aren’t enough or can’t be tolerated. Some patients may eventually switch entirely, but that’s rare and usually only done under close medical supervision.
Do PCSK9 inhibitors cause weight gain or diabetes?
No. Unlike statins, which have a small association with increased blood sugar and type 2 diabetes risk, PCSK9 inhibitors show no effect on weight or glucose metabolism in clinical trials. This makes them a better option for people with prediabetes or metabolic syndrome.
How long do I need to take PCSK9 inhibitors?
Cholesterol management is lifelong. Stopping PCSK9 inhibitors causes LDL to rise back to baseline within weeks. Most patients take them indefinitely, especially if they have heart disease or genetic high cholesterol. The drugs are safe for long-term use-five-year data shows sustained LDL reduction and no new safety concerns.
Are PCSK9 inhibitors safe during pregnancy?
They’re not recommended. There’s no data on their safety in pregnancy, and cholesterol is essential for fetal development. If you’re planning pregnancy, talk to your doctor about switching to safer options like ezetimibe or bile acid sequestrants. Statins are also avoided during pregnancy.
Can I switch from statins to PCSK9 inhibitors on my own?
Absolutely not. Both drugs require medical supervision. Stopping statins abruptly can cause LDL to spike. Starting PCSK9 inhibitors requires insurance approval and proper injection training. Always consult your doctor before changing your treatment plan.
What if I’m afraid of needles?
Many patients are. But most get used to it quickly. The needles are tiny, and the injections are quick. Drugmakers offer free training sessions with nurses. Some patients use auto-injectors that hide the needle. And if needles are a dealbreaker, talk to your doctor about oral alternatives like bempedoic acid or inclisiran (which requires fewer injections).
For many, PCSK9 inhibitors are a lifeline-not because they’re better for everyone, but because they’re the only option that works when statins fail. The goal isn’t to pick one over the other. It’s to find the right tool for your body, your risk, and your life.
Bryan Wolfe
January 13, 2026 AT 08:47Man, I switched from statins to Praluent last year after muscle pain wrecked my workouts-best decision ever. No more feeling like a zombie after grocery shopping. I still take a low-dose statin, but now I can actually lift again. Life’s too short to feel crummy just to lower cholesterol.
Sumit Sharma
January 14, 2026 AT 14:55Statins remain the gold standard due to robust mortality reduction data spanning three decades. PCSK9 inhibitors demonstrate superior LDL-lowering efficacy but lack long-term all-cause mortality evidence. Cost-effectiveness analyses consistently show statins as dominant strategy in primary prevention. Off-label use without documented statin intolerance constitutes medical misallocation.
Jay Powers
January 15, 2026 AT 01:03It’s funny how we treat cholesterol like it’s the enemy when really it’s just a molecule doing its job. The real issue is inflammation and insulin resistance. Statins help with that too, but PCSK9 inhibitors? They’re like a scalpel where statins are a sledgehammer. Neither’s perfect, but at least now we have options that don’t make you feel like you’re aging backward.
Lawrence Jung
January 15, 2026 AT 11:45People think drugs fix problems but they’re just masking symptoms. Your liver makes cholesterol because it’s trying to repair damage. You want to lower LDL? Fix your diet. Stop eating processed junk. Move your body. Take a walk. Stop blaming pills for your laziness. Statins are a crutch. PCSK9 inhibitors? A luxury crutch. The real cure is awareness.
Alice Elanora Shepherd
January 16, 2026 AT 09:19As a registered nurse who’s helped patients navigate this for years, I can confirm: the injection-site reactions are real-but manageable. Most patients adapt within 2–3 weeks. The key is proper technique: rotate sites, use alcohol wipes, and let the pen warm to room temp. And yes, the cost is brutal, but copay cards work if you’re persistent. Don’t give up before you’ve tried.
Christina Widodo
January 16, 2026 AT 11:54Wait, so if I’m on a statin and still have LDL at 120, I’m eligible for PCSK9? What’s the threshold? And does insurance even care if I have fatty liver or just high cholesterol? Also-anyone tried Leqvio? Twice a year sounds like a dream.
Prachi Chauhan
January 17, 2026 AT 17:52My dad took statins for 10 years. Then he got muscle pain so bad he couldn’t climb stairs. We tried PCSK9. He cried the first time he injected himself. But now? He walks 5 miles every morning. No pain. No fog. Just life. Money? We fought the insurance for 4 months. Worth it. You don’t know what peace feels like until you stop feeling broken.
Katherine Carlock
January 18, 2026 AT 13:37Just had my first Leqvio shot last week. Two times a year?? I’m already planning my vacation. No more monthly needles, no more pharmacy runs, no more staring at the $14,000 bill like it’s a horror movie. I still take ezetimibe, but this? This is freedom. Also, the nurse who gave me the shot was so chill she made me laugh. Who knew cholesterol meds could be this chill?
Sona Chandra
January 19, 2026 AT 01:31Ugh, I can’t believe people are still defending statins like they’re holy water. My cousin had a heart attack at 42 because her doctor pushed statins and ignored her muscle pain. She’s on PCSK9 now. She’s alive. Statins nearly killed her. Stop glorifying the old way. New science. New hope. Stop being afraid of change.
Jennifer Phelps
January 19, 2026 AT 14:38Does anyone know if PCSK9 inhibitors affect vitamin D absorption? I’ve been low for years and wonder if it’s the drug or just my diet. Also, any data on long-term bone density? Just curious.
beth cordell
January 19, 2026 AT 14:59