Oxytrol vs Other Oxybutynin Alternatives: Benefits, Side Effects & Cost Comparison
 Oct, 23 2025
Oct, 23 2025
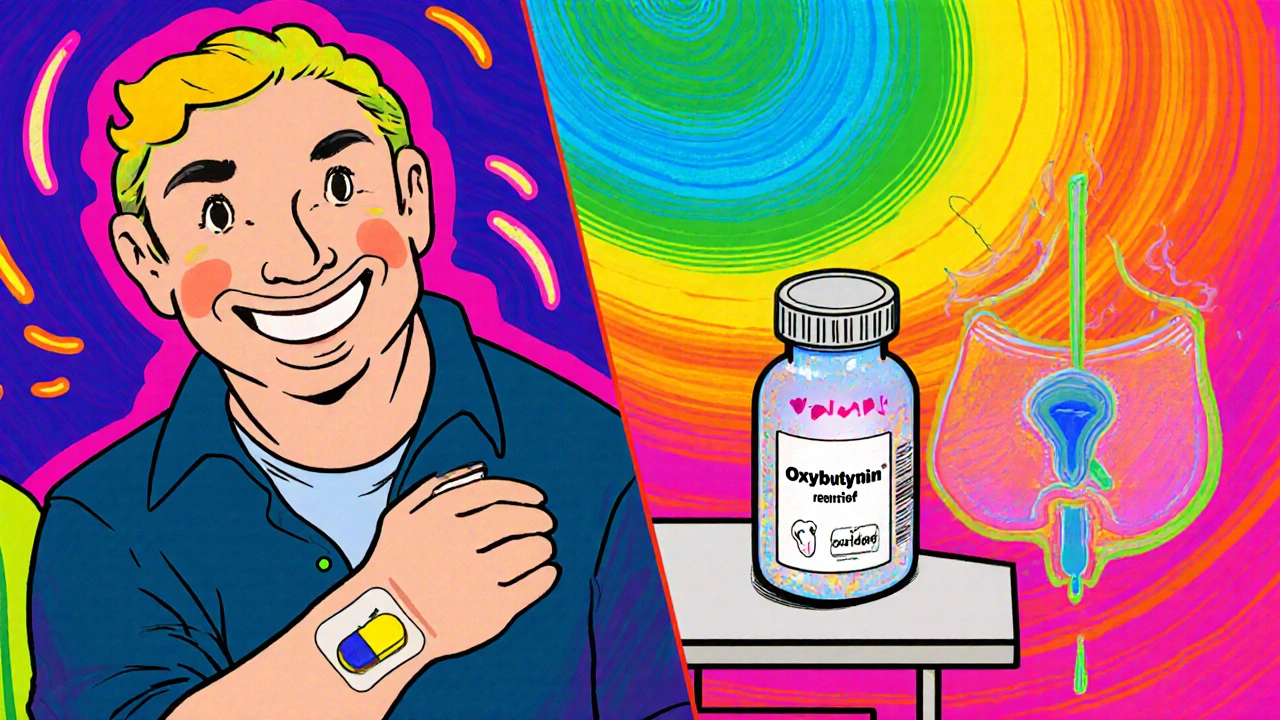
When you’re dealing with overactive bladder (OAB), the number of prescription options can feel overwhelming. One name that often pops up is Oxytrol, a transdermal patch that delivers the anticholinergic drug oxybutynin directly through the skin. But how does it really stack up against the pills, gels, and newer drug classes on the market? This guide walks you through the science, the side‑effect profile, the price tags, and the practical scenarios where each option shines.
What Is Oxytrol and How Does It Work?
Oxytrol is a muscarinic antagonist formulated as a once‑daily skin patch. The active ingredient, oxybutynin, blocks M3 muscarinic receptors in the bladder detrusor muscle, reducing involuntary contractions that cause urgency and frequency. Because it bypasses the gastrointestinal tract, the patch avoids the first‑pass metabolism that triggers many of the classic oral anticholinergic side effects, such as dry mouth and constipation.
Oral Oxybutynin: The Classic Alternative
The original brand-name tablet, Ditropan, and its generic equivalents deliver the same molecule but require multiple daily doses. Oral oxybutynin is absorbed through the gut, leading to higher systemic levels of the drug’s active metabolite N‑desethyloxybutynin. That metabolite is the main culprit behind oral‑related dry mouth, blurred vision, and constipation. For patients who cannot tolerate a patch or who prefer a pill, the oral route remains a viable option.
Other Anticholinergic Options
- Detrol (tolterodine) - a once‑daily tablet with a slightly different receptor affinity profile, often presenting fewer dry‑mouth complaints.
- Toviaz (fesoterodine) - a pro‑drug that converts to an active metabolite similar to tolterodine; dosing can be tailored (4 mg or 8 mg) for symptom severity.
- Enablex (darifenacin) - selective for M3 receptors, which may reduce cognitive side effects in older adults.
All four are oral anticholinergics that share the core mechanism of reducing bladder muscle overactivity, yet their pharmacokinetics differ enough to affect tolerability.
Beta‑3 Agonists: A Different Class
The newest class for OAB is the beta‑3 adrenergic agonist, with Myrbetriq (mirabegron) leading the pack. Instead of blocking muscarinic receptors, mirabegron relaxes the detrusor muscle by stimulating beta‑3 receptors, which can increase bladder capacity without the anticholinergic burden. It’s taken once daily, often in combination with a low‑dose anticholinergic for patients who need extra control.
Key Differences at a Glance
| Drug | Mechanism | Formulation | Typical Dose Frequency | Common Side Effects | UK Approx. Annual Cost (per patient) |
|---|---|---|---|---|---|
| Oxytrol (Oxybutynin) | Muscarinic antagonist (M3) | Transdermal patch | Once daily | Skin irritation, mild dry mouth | £180‑£250 |
| Ditropan (Oxybutynin) | Muscarinic antagonist (M3) | Oral tablet | 2‑3 times daily | Dry mouth, constipation, blurred vision | £80‑£120 |
| Detrol (Tolterodine) | Muscarinic antagonist (M2/M3) | Oral tablet | Once or twice daily | Dry mouth, headache | £110‑£160 |
| Enablex (Darifenacin) | Muscarinic antagonist (M3 selective) | Oral tablet | Once daily | Dry mouth, constipation, CNS effects (rare) | £130‑£190 |
| Myrbetriq (Mirabegron) | Beta‑3 adrenergic agonist | Oral tablet | Once daily | Hypertension, nasopharyngitis, headache | £210‑£280 |
When Might You Choose Oxytrol?
Oxytrol shines for patients who struggle with the classic anticholinergic side effects seen with oral tablets. Because the drug bypasses the liver, the metabolite that causes dry mouth is produced in much lower amounts. If you’ve tried oral oxybutynin and found it intolerable, the patch can often restore symptom control without the same gastrointestinal complaints.
Other scenarios where the patch is advantageous include:
- Difficulty swallowing pills - the adhesive strip is a hands‑free solution.
- Need for consistent plasma levels - the patch provides a steady release over 24 hours.
- Older adults with polypharmacy - fewer drug‑drug interactions compared to oral agents.

When Might Alternatives Be Better?
If cost is a primary concern, generic oral oxybutynin remains the cheapest option, even after the NHS prescription charge is accounted for. For patients with skin sensitivities, the patch could trigger dermatitis, making an oral route preferable.
Beta‑3 agonists like Myrbetriq are worth considering when anticholinergic side effects are prohibitive, especially in people with narrow‑angle glaucoma or severe cognitive impairment. Some clinicians start with a low‑dose mirabegron and add a low‑dose anticholinergic (often detrol or oxytrol) if urgency persists.
Practical Tips for Switching or Starting Therapy
- Assess baseline bladder diary - record frequency, volume, and nighttime voids for three days.
- Identify contraindications - skin allergies (patch), uncontrolled hypertension (mirabegron), or narrow‑angle glaucoma (any anticholinergic).
- Choose the first line based on side‑effect tolerance:
- Patch for dry‑mouth avoidance.
- Oral for cost‑sensitivity.
- Beta‑3 agonist for cognitive safety.
- Initiate at the lowest effective dose - most tablets start at 5 mg (oxybutynin) or 2 mg (tolterodine).
- Re‑evaluate after 4‑6 weeks using the bladder diary; adjust dose or switch class as needed.
Always discuss any changes with your GP or urologist, especially if you have comorbidities like diabetes or Parkinson’s disease that can affect bladder function.
Key Takeaways
- Oxytrol delivers oxybutynin via skin, reducing oral‑related dry‑mouth side effects.
- Oral anticholinergics (Ditropan, Detrol, Enablex, Toviaz) remain effective and cost‑friendly but come with classic gastrointestinal complaints.
- Myrbetriq offers a non‑anticholinergic route, useful for patients where cognitive or visual side effects are a concern.
- Cost, tolerability, comorbidities, and patient preference drive the final choice.
Can I use Oxytrol if I’m already on another OAB medication?
Switching directly is possible, but you should taper the oral drug over a few days to avoid overlapping anticholinergic effects. Always follow your prescriber’s taper schedule.
What should I do if the Oxytrol patch causes skin irritation?
Remove the patch, clean the area with mild soap, and apply a hypoallergenic barrier cream. If irritation persists after 48 hours, consult your doctor for an alternative formulation.
Is mirabegron safe for people with high blood pressure?
Mirabegron can raise systolic pressure by up to 4‑5 mmHg. If you have uncontrolled hypertension, your doctor may prefer an anticholinergic or a lower dose of mirabegron combined with an anticholinergic.
How quickly does the Oxytrol patch start working?
Therapeutic levels are reached within 24‑48 hours, but most patients notice a reduction in urgency after about a week of consistent use.
Can I combine an anticholinergic with mirabegron?
Yes, many guidelines, including NICE, endorse combination therapy for refractory OAB. Starting at low doses of each drug reduces the risk of side effects while providing synergistic symptom control.
Dante Russello
October 23, 2025 AT 12:23If you're navigating the maze of over‑active bladder treatments, the Oxytrol patch is worth a deep dive-because it flips the script on classic anticholinergic side effects, especially the dreaded dry mouth that can feel like a desert in your mouth!!!; The transdermal route sidesteps first‑pass metabolism, meaning the nasty metabolite N‑desethyloxybutynin stays low, which translates to fewer gastrointestinal complaints; for patients who have tried oral oxybutynin and coughed up a storm of constipation and blurred vision, the patch offers a steadier plasma level that mimics a controlled release infusion; it also dries out the skin a bit, but most users report only mild irritation that can be managed with barrier creams or rotating sites; another upside is the once‑daily application-no more juggling multiple doses throughout the day, which improves adherence especially in older adults juggling many meds; cost‑wise, the patch sits higher than generic tablets in the UK (£180‑£250 versus £80‑£120), but the trade‑off may be worthwhile if you value quality‑of‑life gains; clinicians often start patients on the lowest patch strength and assess after a week, looking for reductions in urgency episodes in the bladder diary; remember to record baseline voiding frequency for three days before initiating therapy, so you have a clear before‑and‑after picture; if skin sensitivity becomes an issue, rotate the patch location and keep the area clean-no harsh soaps, just mild cleanser and a breath of air; for those on polypharmacy regimens, the patch reduces drug‑drug interaction potential because it bypasses the gut and liver pathways; some insurers may require step therapy, so document the intolerance to oral forms meticulously; the patch reaches therapeutic levels within 24‑48 hours, but many patients notice a meaningful decline in nocturia after about a week of consistent use; baseline blood pressure should be checked, although the patch has minimal impact there compared to beta‑3 agonists; if you have narrow‑angle glaucoma, the patch is still safer than oral anticholinergics, but always loop in your ophthalmologist; finally, the patch can be combined with a low‑dose beta‑3 agonist like mirabegron for refractory cases, but do so under close supervision to avoid additive hypertension; overall, Oxytrol shines when you need to dodge dry mouth, want stable drug delivery, and can manage a modest skin reaction-making it a solid option in the OAB arsenal.
James Gray
October 23, 2025 AT 13:46Wow, great breakdown! i totally get why the patch could be a game‑changer for folks who cant swallow pills or hate that dry‑mouth feeling. the price might be a bit higher but think about the peace of mind and less bathroom trips-totally worth it for many! keep sharing these deets, it helps a lot of us decide what to ask our docs about.
Scott Ring
October 23, 2025 AT 15:10Appreciate the thorough info. For anyone juggling meds, the steady release of the patch can cut down on peaks and troughs. Just make sure to rotate the site to keep skin irritation low.
Shubhi Sahni
October 23, 2025 AT 16:33Indeed, the steady plasma concentration is a major benefit!!!; Moreover, the patch eliminates the gastrointestinal load, reducing constipation risk!!!; For patients with multiple co‑morbidities, fewer drug‑drug interactions are a clear advantage!!!; Always counsel on proper application technique to maximize adherence and minimize skin irritation!!!.
Danielle St. Marie
October 23, 2025 AT 17:56Honestly, the patch is overrated-American pharma loves to push pricey transdermals while cheap generics sit on shelves. 🇺🇸💊 If you’re smart, you’ll stick to oral oxybutynin and save your money for something that truly matters. 🙄💸
keerthi yeligay
October 23, 2025 AT 19:20i think both side have point. patch helps dry mouth but cost high. oral is cheap but side effects. each patien need decide.
Peter Richmond
October 23, 2025 AT 20:43Thanks for the balanced overview. Patients should weigh efficacy, side‑effect profile, and personal preferences when selecting therapy.
Bonnie Lin
October 23, 2025 AT 22:06Great summary-very helpful.