Myofascial Pain Syndrome: Trigger Points and How to Release Them
 Dec, 9 2025
Dec, 9 2025
Chronic muscle pain that won’t go away-even after rest, ice, or painkillers-might not be a strain, a pinched nerve, or arthritis. It could be myofascial pain syndrome (MPS), a hidden culprit behind many persistent aches. Unlike general soreness, MPS comes from specific knots in your muscles called trigger points. These aren’t just tender spots; they’re hyperactive zones that send pain signals to other parts of your body, making it easy to misdiagnose. You might think your headache is from stress, your shoulder pain is from typing too long, or your jaw ache is from grinding your teeth. But if the pain keeps coming back in the same patterns, it could be your muscles talking in code.
What Exactly Are Trigger Points?
Trigger points are tiny, tight bands of muscle fiber, usually 2 to 10 millimeters across, that feel like little marbles under your skin. They form when muscle fibers stay locked in contraction, often because of injury, overuse, or poor posture. Think of it like a knot in a rope-you can’t just pull harder to fix it. The muscle is stuck, and that tension cuts off blood flow, creating a chemical soup of pain-causing substances like acetylcholine, serotonin, and acid. The pH in these spots drops to around 4.3, which is as acidic as a lemon. That’s why pressing on them hurts so much-and why the pain often spreads. There are two types: active and latent. Active trigger points hurt on their own. You don’t even need to touch them. You feel the ache in your neck, your shoulder, or even your tooth. Latent ones only hurt when you press on them. But they’re still trouble-they can become active again if you get stressed, sleep poorly, or sit slouched at your desk for too long. The most common muscles affected? The upper trapezius (that ridge from your neck to your shoulder), the levator scapulae (running down the side of your neck), and the temporalis (in your temples). These are the muscles that tense up when you’re stressed, hunched over a screen, or clenching your jaw. Studies show over 65% of people with chronic muscle pain have trigger points in these areas.How Is It Different From Fibromyalgia?
A lot of people confuse myofascial pain syndrome with fibromyalgia. They both involve pain, but they’re not the same. Fibromyalgia causes widespread, symmetric pain all over the body-both sides of your neck, back, hips, knees. It’s more about sensitivity than knots. Trigger points, on the other hand, are local. You can find them. You can press on them. And they refer pain in predictable patterns. Press a trigger point in your trapezius, and you’ll feel pain near your ear or temple. Press one in your gluteus medius, and your hip or thigh might throb. That’s not random. That’s a map. Doctors used to think fibromyalgia and MPS were the same. But research shows they’re separate. One key difference: trigger points cause a local twitch response. If you press just right, the muscle fiber jumps. That doesn’t happen with fibromyalgia’s tender points. Also, trigger points can be treated and often resolved. Fibromyalgia is a central nervous system condition-harder to reverse.Why Do Trigger Points Form?
It’s not just about being lazy or sitting too long. Trigger points develop from a mix of physical, chemical, and lifestyle factors:- Acute injury: A car accident, fall, or sports trauma can set off trigger points. Up to 70% of people with whiplash develop MPS within weeks.
- Chronic posture: Forward head posture-common with phone and computer use-makes your upper traps work overtime. Studies show this increases trigger point risk by 3 to 5 times.
- Structural issues: A leg length difference of more than 1 cm? That throws off your pelvis and spine. Risk of MPS goes up by 40%.
- Nutrition and hormones: Low vitamin D (under 20 ng/mL) is linked to 60% higher MPS rates. Hypothyroidism shows up in 15-25% of chronic cases.
- Stress: When you’re anxious, your muscles stay tight. No relaxation. No recovery. Just constant tension.
How Do You Find a Trigger Point?
Finding trigger points isn’t magic. It’s skill. A trained therapist will feel for taut bands in your muscles, then press slowly. If you feel pain right there-and it radiates to another spot-that’s a trigger point. The gold standard is the local twitch response: a quick, involuntary spasm when the point is pressed. It’s not always visible, but you’ll feel it. But here’s the problem: not all providers know how to do this right. Studies show inter-rater reliability varies wildly-from poor to excellent-depending on training. Some therapists miss them. Others press too hard. That’s why so many people say, “I had trigger point therapy and it didn’t help.” They didn’t get the right treatment.
Proven Ways to Release Trigger Points
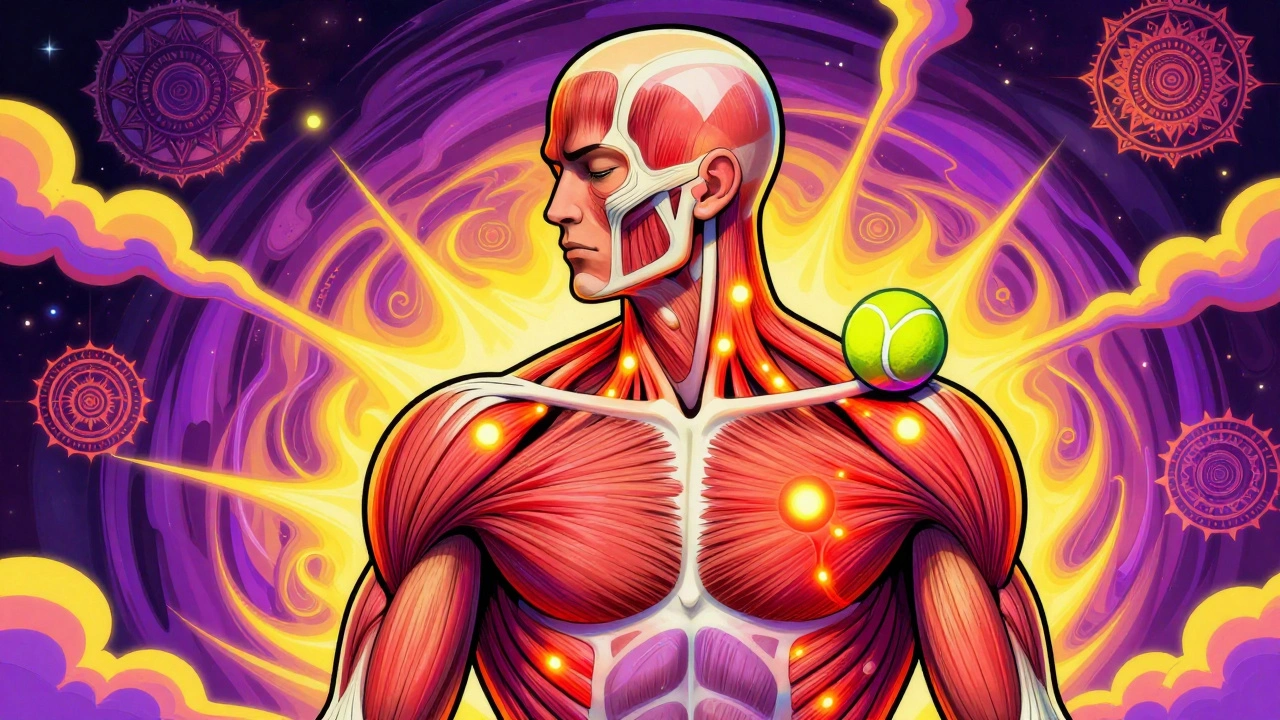
There’s no one-size-fits-all fix, but several techniques have strong evidence behind them:Ischemic Compression
This is the simplest and most accessible method. You press directly on the trigger point with your thumb, knuckle, or a tennis ball. Hold for 30 to 90 seconds, until the pain eases by about 50%. Then release slowly. Repeat 2-3 times. Do this daily. It’s low-tech, cheap, and works for 60-75% of people in the short term.- For upper traps: Lean against a wall with a tennis ball between your shoulder blade and spine. Roll slowly until you find the knot.
- For temporalis: Use your index finger to press along your temple, just above your jawline. Hold until the ache softens.
Dry Needling
This is when a therapist inserts thin needles into the trigger point-no medicine, just the needle. It often causes a twitch. Studies show 65-80% of patients get relief that lasts 4 to 12 weeks. It’s not acupuncture. It’s a targeted muscle intervention. The needles reset the muscle’s electrical activity. It’s not painless, but it’s fast. Most people feel better within 24-48 hours.Trigger Point Injections
A small amount of lidocaine (a numbing agent) is injected directly into the trigger point. It gives immediate relief-70-85% of patients report pain dropping within minutes. But the effect fades after 2-8 weeks. A Cochrane Review found no real difference between lidocaine injections and dry needling at the 4-week mark. So if you’re avoiding needles, dry needling is just as effective.Spray and Stretch
This is a classic technique. A cold spray (like ethyl chloride) is sprayed over the area where the pain is referred-say, your shoulder or head-then the muscle is gently stretched. The cold numbs the skin and tricks the nervous system, making stretching easier. Works best for neck and jaw pain. About 50-65% effective.Instrument-Assisted Soft Tissue Mobilization (IASTM)
Therapists use metal or plastic tools to scrape along the muscle. It breaks up adhesions and stimulates blood flow. Good for stubborn knots that don’t respond to pressure alone. Success rates: 55-70%.Low-Level Laser Therapy (LLLT)
A non-invasive option using specific wavelengths of light (808-905 nm). It reduces inflammation and helps muscle cells recover. Not a quick fix, but useful for people who can’t tolerate pressure or needles. Studies show 40-60% pain reduction after 6-8 sessions.Why Do Symptoms Come Back?
Even if you get relief, MPS often returns. Why? Because the root causes are still there. A study of over 1,200 patients found that those who did a combination of manual therapy, dry needling, and daily home stretches saw a 65% drop in pain at 12 weeks. Those who didn’t stick with home care? Only 35% improvement. And 40-60% of people had symptoms return within six months without maintenance. The key is consistency. You can’t just treat the trigger point and forget about your posture, your sleep, your stress levels. If you’re still hunched over your laptop for 8 hours a day, the knots will come back. If you’re low on vitamin D, your muscles won’t recover properly.What You Can Do at Home
You don’t need to see a specialist every week. Here’s a practical daily plan:- Self-massage: Use a tennis ball or foam roller for 10-15 minutes a day. Focus on your upper back, neck, and jaw.
- Heat before stretching: Apply a warm towel or heating pad (40-45°C) for 15 minutes before stretching. Heat relaxes the muscle, making stretches safer and more effective.
- Posture checks: Set a timer to check your posture every hour. Shoulders down, chin slightly tucked, screen at eye level.
- Stretch daily: Do 3 sets of 10 reps of neck retractions, shoulder rolls, and chin tucks-twice a day.
- Check your vitamin D: Get a blood test if you’re constantly tired or sore. Many people with chronic pain are deficient.
When to See a Professional
If you’ve tried home care for 4-6 weeks and your pain hasn’t improved-or it’s getting worse-it’s time to see someone trained in myofascial therapy. Look for a physical therapist, chiropractor, or sports medicine doctor with certification in trigger point therapy. The American Academy of Physical Medicine and Rehabilitation offers a 40-hour certification program. Ask if they’ve trained with Travell and Simons’ methods or use the Trigger Point Therapy Workbook as a reference. Avoid providers who just “massage” without identifying specific trigger points. You need precision, not pressure.The Bigger Picture
Myofascial pain syndrome is one of the most common-but least understood-causes of chronic pain. It’s responsible for nearly a third of all musculoskeletal visits to primary care doctors. And because it’s not visible on X-rays or MRIs, it’s often missed. That’s why people end up with unnecessary scans, nerve blocks, or even surgery. The good news? MPS responds well to non-drug treatments. In fact, with the opioid crisis, non-pharmacological options like trigger point therapy have grown 200% since 2015. It’s not a fringe practice anymore. It’s becoming central to pain management. You don’t have to live with pain that feels like it’s coming from nowhere. The trigger points are real. The relief is possible. It just takes knowing where to look-and how to release them.Can trigger points be seen on an MRI or X-ray?
No, trigger points cannot be seen on standard imaging like MRI, X-ray, or CT scans. They’re functional, not structural-they’re areas of abnormal muscle activity and biochemical changes, not tissue damage or bone misalignment. That’s why many people get misdiagnosed; doctors order scans looking for a structural problem and find nothing. Diagnosis relies on physical examination: finding taut bands, localized tenderness, referred pain, and a local twitch response.
Is dry needling the same as acupuncture?
No. Acupuncture is based on traditional Chinese medicine and targets energy pathways called meridians. Dry needling is a Western medical technique that targets specific trigger points in muscles. The needles are inserted for the same reason: to release muscle tension-but the theory, placement, and training behind them are completely different. Dry needling is taught in physical therapy and medical schools; acupuncture requires separate licensing.
How long does it take to see results from trigger point therapy?
Some people feel relief within hours-especially after dry needling or trigger point injections. With self-care like ischemic compression, it may take 3-7 days of consistent daily work to notice a difference. For lasting results, most people need 4-6 sessions over 2-4 weeks, combined with home exercises. Chronic cases may take longer, but improvement usually starts within the first two weeks.
Can stress cause trigger points?
Yes. Stress triggers the body’s fight-or-flight response, which keeps muscles tense. Over time, this constant tension leads to muscle fatigue and the formation of trigger points. People under chronic stress are far more likely to develop MPS, especially in the neck, shoulders, and jaw. Managing stress through sleep, breathing exercises, or therapy isn’t just helpful-it’s essential for long-term relief.
Why does my pain move around?
That’s referred pain-a hallmark of trigger points. A knot in your upper trapezius might cause pain in your temple, ear, or even your hand. A trigger point in your gluteus medius can mimic sciatica. The pain doesn’t move because the problem is moving-it’s because the nerve pathways from that muscle send signals to distant areas. Once the trigger point is released, the referred pain stops. That’s why mapping your pain patterns is so important for diagnosis.
Are trigger point injections painful?
There’s a brief sting when the needle goes in, followed by a deep ache as the trigger point is activated. Many people describe it as a “good hurt”-like when a massage hits the right spot. The discomfort lasts only seconds. The numbing effect of lidocaine kicks in quickly, and most people report significant relief within minutes. If you’re anxious about needles, dry needling or ischemic compression are equally effective alternatives.
Next Steps: What to Do Today
If you’ve been living with unexplained muscle pain:- Find one area where you feel a knot-probably your neck, shoulder, or upper back.
- Use a tennis ball or your fingers to apply steady pressure for 60 seconds. Breathe through it.
- Notice if the pain spreads to another spot. That’s a sign of a trigger point.
- Do 10 minutes of self-massage daily for a week.
- Check your vitamin D levels with your doctor if you’re still sore after a few weeks.
Ben Greening
December 10, 2025 AT 17:45Interesting breakdown of trigger points and their mechanisms. The biochemical explanation-especially the pH drop to 4.3-is both startling and convincing. It’s rare to see such a clear link between muscle physiology and systemic pain patterns in lay-accessible material.
That said, the emphasis on self-care is well-placed. Many patients overlook the fact that trigger points are often symptoms, not root causes.
One minor quibble: the section on dry needling could have mentioned the importance of sterile technique and practitioner credentialing. Not all clinics adhere to the same standards.
Nikki Smellie
December 11, 2025 AT 20:39Have you considered that trigger points are not natural at all? They are a direct result of government-mandated EMF exposure from 5G towers, which disrupts cellular calcium channels and causes involuntary muscle contractions. The pharmaceutical industry suppresses this truth because they profit from painkillers and injections. Look at the timing: MPS diagnoses spiked right after cell towers were installed in every neighborhood.
Also, vitamin D deficiency? That’s a distraction. The real culprit is fluoride in the water-fluoride binds to magnesium, which is needed for muscle relaxation. Drink spring water. Stop trusting the FDA.
:-)
Stephanie Maillet
December 12, 2025 AT 22:58There’s something profoundly poetic about the body speaking in code… and we, in our modern haste, have forgotten how to listen.
Trigger points aren’t just knots-they’re silent pleas from tissues that have been asked to endure too much, for too long, without rest.
It’s not merely about posture or vitamin D… it’s about the rhythm of our lives. We rush. We tense. We don’t pause. And the body, in its quiet wisdom, begins to lock itself up-like a violin string that’s been tuned too tight for too long.
Perhaps the real therapy isn’t the needle, or the ball, or the spray… but the permission to slow down.
And yet… we’re afraid to.
What if healing begins not with pressure… but with presence?
David Palmer
December 13, 2025 AT 21:45Bro, I’ve had this pain in my neck for years. Tried everything. Massage? Nah. Heat? Meh. Then I just started rolling a lacrosse ball on my traps while watching Netflix. Boom. 80% better in a week.
Don’t overthink it. Your body’s not a mystery. It’s just tired.
Also, stop sitting like a zombie at your desk. Stand up. Stretch. Breathe. Do it now.
Doris Lee
December 15, 2025 AT 05:57This is exactly the kind of info I wish I’d had five years ago. If you’re reading this and you’ve been told ‘it’s all in your head’-you’re not crazy. Your muscles are screaming.
Start with the tennis ball. Just five minutes a day. You don’t need a degree or a fancy clinic. You just need consistency.
And hey-you’re not alone. We’ve all been there. You’ve got this.
Michaux Hyatt
December 16, 2025 AT 12:12Great summary. I’d add one thing: the local twitch response is the golden diagnostic tool. If you don’t get a twitch when you press, you’re not on the trigger point. Many people press too hard or too fast and miss it.
Also, don’t underestimate the power of diaphragmatic breathing during self-massage. It helps the nervous system switch from fight-or-flight to rest-and-digest, which makes the muscle more receptive to release.
And yes-vitamin D matters. Get tested. I’ve seen patients improve dramatically after correcting a 12 ng/mL level.
Raj Rsvpraj
December 18, 2025 AT 02:20Of course you Westerners are only now discovering this. In India, Ayurvedic practitioners have understood myofascial tension for over 5,000 years. We call it ‘vata imbalance’-and we treat it with abhyanga oil massage, heat, and breathwork. You moderns think you invented pain management? Ha.
Also, your ‘dry needling’? That’s just a watered-down version of acupuncture. We did it before your ancestors were wearing animal skins.
And your ‘tennis ball’? We used walnut shells. More precise. More effective.
Stop acting like this is new. It’s not innovation-it’s appropriation.
Frank Nouwens
December 18, 2025 AT 03:19The distinction between MPS and fibromyalgia is critical and often overlooked in clinical practice. The referred pain patterns are highly reproducible and follow anatomical maps first documented by Travell and Simons in the 1980s. These are not arbitrary.
Furthermore, the efficacy of ischemic compression is supported by multiple randomized controlled trials, including a 2021 meta-analysis in the Journal of Orthopaedic & Sports Physical Therapy.
It is unfortunate that non-pharmacological interventions remain underutilized in primary care settings, despite their cost-effectiveness and low risk profile.
Michelle Edwards
December 18, 2025 AT 12:22I’ve been living with this for over a decade. I thought it was arthritis. Then migraines. Then stress. Turns out, it was just my upper traps screaming for mercy.
Started with the tennis ball. Did it every morning before coffee. Didn’t even tell anyone. Just me, the wall, and 10 minutes of quiet.
It’s not glamorous. But it works.
And honestly? That quiet time became the most healing part.
Neelam Kumari
December 20, 2025 AT 10:48Wow. Another ‘self-care’ miracle cure for people who refuse to see a real doctor. You know what? Most of you don’t even know what a trigger point is-you just Google ‘neck pain’ and buy a foam roller.
And vitamin D? Please. That’s the new placebo. You think your pain is from low vitamin D? Maybe it’s from a herniated disc, or nerve entrapment, or a tumor.
Stop self-diagnosing. Go get an MRI. Or at least, stop pretending a tennis ball is medicine.
Queenie Chan
December 21, 2025 AT 03:37Trigger points are like emotional ghosts-tucked into muscle tissue, whispering old fears, old trauma, old hours spent hunched over screens like penitents in a digital monastery.
That twitch response? That’s the muscle gasping, ‘I remember!’
And the fact that we need a needle or a ball to make it speak? That’s the tragedy.
We’ve forgotten how to touch each other. How to rest. How to let go.
So we press. We poke. We spray.
But maybe… just maybe… the real release comes when we finally stop running from the silence inside our own bodies.
Jack Appleby
December 22, 2025 AT 19:33While the general overview is serviceable, the piece exhibits a distressing lack of nuance regarding the pathophysiology of trigger points. The assertion that ‘pH drops to 4.3’ is misleading; while local acidosis occurs, the extracellular pH rarely falls below 6.5 in vivo, even in ischemic tissue. The cited value appears to be an artifact of in vitro models or misinterpreted microdialysis data.
Additionally, the conflation of dry needling with ‘Western medical technique’ ignores the fact that modern dry needling evolved directly from acupuncture theory-specifically, the ‘ashi point’ concept. The distinction is semantically convenient but historically inaccurate.
Finally, the recommendation to use a tennis ball for temporalis release is biomechanically unsound; the temporalis is a deep, cranial muscle. Finger pressure is the only safe modality. Recommending a ball here is not merely ineffective-it’s potentially injurious.