How to Teach Family Members to Recognize Overdose Symptoms
 Dec, 4 2025
Dec, 4 2025
Every year, more than 100,000 people in the U.S. die from drug overdoses-and nearly 8 out of 10 of those happen at home. That means the person who’s most likely to save a life during an overdose isn’t a paramedic. It’s a sibling, a parent, a partner, or a child. If someone you love uses drugs-even occasionally-teaching your family how to spot an overdose could mean the difference between life and death.
What an Overdose Really Looks Like
Many people think someone overdosing is just really drunk or high. That’s not true. An overdose means the body can’t keep up. Breathing slows down or stops. The brain isn’t getting oxygen. Minutes matter. For opioids like heroin, fentanyl, or prescription painkillers, there are three clear signs: unresponsiveness, slow or no breathing, and blue or gray lips and fingernails. This is called the opioid triad. But there are other clues too: the person might be limp, like a ragdoll. Their skin might feel cold and clammy. You might hear a gurgling sound-like they’re drowning in their own saliva. That’s not just being sick. That’s their airway closing. For stimulants like cocaine or meth, the signs are different. The person might be sweating heavily, shaking, or having a seizure. Their heart races. Their body temperature soars past 104°F. They might panic, scream, or become violent. It looks like a medical emergency-and it is. The biggest mistake? Assuming they’ll wake up if you shake them. If they don’t respond to a sternum rub (firmly rubbing the center of their chest with your knuckles), they’re not just passed out. They’re overdosing. And time is running out.Why Family Training Works-And Why It’s Not Optional
Studies show that when family members are trained, overdose deaths drop by up to 40%. Why? Because they’re already there. Emergency services take 8 to 10 minutes to arrive. In that time, a person can die. Training isn’t about scaring people. It’s about giving them tools. A 2023 study of over 2,800 families found that those who practiced with training kits were 89% more likely to remember what to do three months later. Those who only watched videos? Only 42% remembered. Real families say the same thing: “I didn’t think I’d ever need this.” Then they used it. One father in Ohio reversed his son’s overdose with Narcan after practicing with a training kit three times. He said, “I knew exactly what to do because I’d done it before-not in my head, but with my hands.”How to Teach It: The Recognize-Respond-Revive Method
The best training doesn’t just tell people what to do. It lets them do it. Use this three-step method:- Recognize - Teach the signs. Use photos or videos that show different skin tones. Blue lips on fair skin look different than grayish skin on darker skin. Many people miss overdoses because they’re only taught to look for one color change. Show them both.
- Respond - Show them how to call 911. Tell them to say, “I think someone is overdosing. They’re not breathing.” Don’t let them hesitate. Emphasize: 911 won’t arrest them. In 31 states, Good Samaritan laws protect people who call for help.
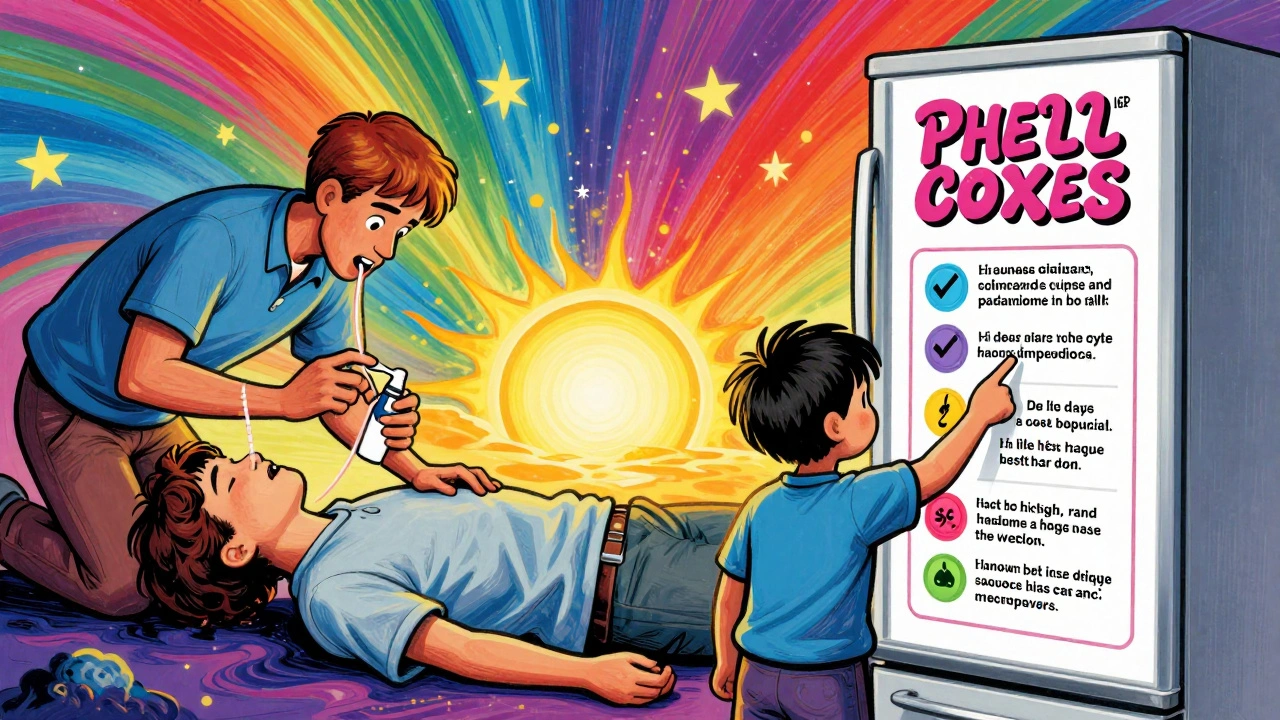
- Revive - Practice giving naloxone. Use a training device that looks and feels like the real thing. There’s no needle. Just spray one dose into each nostril. Then, give rescue breaths-two every five seconds-until help arrives or they wake up.
What You Need to Get Started
You don’t need a clinic or a doctor. Here’s what you need at home:- Two naloxone training kits (around $35 each). These are identical to the real thing, but won’t deliver medicine. They’re used for practice.
- A mannequin or even a pillow to practice rescue breathing on.
- Printed cards with the signs of overdose-put one on the fridge.
- A skin tone guide. The CDC and California Health Department offer free ones online. Print them.
What to Do If Someone Overdoses
If you ever need to act:- Shout their name. Shake their shoulder. Rub their sternum hard with your knuckles. If they don’t respond, assume overdose.
- Call 911. Say: “Overdose. Not breathing.” Don’t hang up.
- Give one dose of naloxone in each nostril. Push the plunger all the way in.
- Start rescue breathing: tilt the head back, lift the chin, pinch the nose, give two breaths every five seconds.
- If they don’t wake up in 3 minutes, give a second dose of naloxone.
- Stay with them. Even if they wake up, they can crash again. Wait for EMS.
Common Mistakes and How to Avoid Them
Families often make these errors:- Waiting to see if they “snap out of it.” Don’t. Every minute without oxygen kills brain cells.
- Thinking naloxone is a cure-all. It only works on opioids. It won’t help with cocaine or meth. But it still needs to be given-because many overdoses involve mixed drugs.
- Being afraid to use it. Naloxone is safe. Even if they didn’t overdose, it won’t hurt them.
- Not practicing. Stress makes you forget. Practice twice. Once with the training kit, once with a friend playing the role of the person overdosing.

How to Talk About It Without Scaring People
This is hard. People feel guilty. They think talking about overdose means they’re giving up on their loved one. That’s not true. Talking about it means you’re fighting for them. Try this: “I love you. I don’t want to lose you. If something happens, I want to know what to do. Let’s learn together.” Don’t make it a lecture. Make it a family safety plan-like fire drills. Keep the training kits with your first aid supplies. Put the card on the fridge. Practice once every few months.What Happens After You Save a Life
Surviving an overdose doesn’t mean the crisis is over. The person might need medical care, counseling, or detox. But they’re alive. That’s the first step. Many families report feeling empowered after training. One mother in Georgia said: “I used to feel helpless. Now I know I can act. That changed everything.” The goal isn’t to fix addiction. The goal is to keep someone alive until they’re ready to get help.Can I get naloxone without a prescription?
Yes, in 31 states, you can walk into a pharmacy and ask for naloxone without a prescription. In 19 states, you need to complete a short training first. Check your state’s health department website or call your local pharmacy. Many offer free kits.
What if I’m not sure it’s an overdose?
If someone is unresponsive, not breathing normally, or turning blue/gray, give naloxone anyway. It’s safe. It won’t hurt someone who hasn’t overdosed on opioids. Waiting to be sure could cost their life.
Does naloxone work on fentanyl?
Yes. Fentanyl is 50 to 100 times stronger than heroin, and it’s in most illegal pills now. One dose of naloxone might not be enough. If the person doesn’t wake up after 3 minutes, give a second dose. Keep giving rescue breaths until help arrives.
Can I train kids or teens?
Yes. Teens as young as 12 can learn to recognize signs and use naloxone. Many schools and youth programs now offer training. Use simple language, practice with a mannequin, and make it part of family safety rules-like knowing where the fire extinguisher is.
Is there a mobile app for overdose training?
Yes. The Overdose Lifeline app (free on iOS and Android) has step-by-step video guides, a location finder for free naloxone, and a timer to help you track rescue breathing. It’s been downloaded over 147,000 times and used in real emergencies across the U.S.
What if I’m scared to talk about this with my family?
It’s normal. Many people feel like they’re tempting fate. But the people who wait until it’s too late are the ones who never talked about it. Start small: “I read something important. Can we watch a 5-minute video together?” Most families say once they do, they feel stronger-not scared.
Mellissa Landrum
December 4, 2025 AT 16:19Mark Curry
December 6, 2025 AT 04:03simple tools, simple acts. that's all it takes.
Annie Grajewski
December 7, 2025 AT 05:44Mark Ziegenbein
December 7, 2025 AT 07:03Marvin Gordon
December 7, 2025 AT 14:32ashlie perry
December 9, 2025 AT 07:44Stephanie Fiero
December 9, 2025 AT 23:33Laura Saye
December 10, 2025 AT 09:42Michael Dioso
December 10, 2025 AT 21:56Krishan Patel
December 10, 2025 AT 22:21Manish Shankar
December 12, 2025 AT 18:22Mark Curry
December 13, 2025 AT 23:57