How to Read Prescription Labels to Avoid Dangerous Drug Interactions
 Dec, 3 2025
Dec, 3 2025
Every time you pick up a prescription, the label on the bottle holds life-or-death information. But most people skim it like a receipt-glancing at the name, the dose, and maybe the number of pills. That’s not enough. Prescription label information is designed to stop dangerous drug interactions before they happen. And if you don’t know how to read it, you’re putting yourself at risk.
Every year in the U.S., about 2 million people have bad reactions to medications because of interactions they didn’t see coming. Of those, 100,000 end up in the hospital. Many of these cases are preventable. The FDA requires every prescription label to include clear, standardized warnings about interactions. But unless you know where to look and what to look for, those warnings might as well be invisible.
Where to Find Drug Interaction Warnings on Your Label
Prescription labels aren’t random text. They follow strict FDA rules. The most important section for avoiding interactions is called Drug Interactions-usually labeled as Section 7. This isn’t buried in fine print. It’s a dedicated part of the label, right after the dosage instructions and before the side effects.
Here’s what to expect in that section:
- "Avoid concomitant use of [Drug A] with [Drug B]" - This means don’t take them together. Ever. This is a hard stop.
- "Reduce dosage of [Drug A] when used with [Drug B]" - You can still take both, but the dose of one needs to be lowered to stay safe.
- "Monitor for [symptom]" - Like dizziness, bleeding, or irregular heartbeat. If you notice this, call your doctor right away.
Don’t ignore the Warnings and Precautions section (Section 5). This is where the FDA requires the most serious interaction warnings to appear-especially those that could lead to death or hospitalization. If your label says something like "Concomitant use may cause fatal respiratory depression," that’s not a suggestion. It’s a red alert.
And don’t forget over-the-counter (OTC) meds. The "Warnings" section on ibuprofen, cold medicine, or sleep aids often lists interactions too. A 2023 study found that 98% of OTC products include critical interaction info-but only 57% of people actually read it.
What the Warnings Really Mean (Plain Language)
Pharmaceutical labels use legal and medical language that can sound like a foreign language. Here’s how to decode the most common phrases:
- "Concomitant use" = Taking two or more drugs at the same time.
- "Significant interaction" = This combo can make one drug stronger, weaker, or cause a dangerous side effect.
- "CYP3A4 substrate/inhibitor/inducer" = This is about how your liver processes the drug. If you’re not a doctor, just look for the plain English warning below it. The FDA now requires this to be followed by simple language like "May increase risk of bleeding" or "May reduce effectiveness of birth control."
- "Use with caution" = Proceed, but watch for symptoms. Don’t assume it’s safe just because it’s not "avoid."
Here’s a real example from a common blood thinner, warfarin: "Avoid concomitant use with ginkgo biloba. May increase risk of bleeding." Many people take ginkgo for memory, not realizing it’s a herbal supplement with the same danger level as a prescription drug. And here’s the kicker: only 17% of prescription labels even mention herbal supplements-even though they cause 32% of serious interactions.
Why You Can’t Rely on Apps Alone
There are dozens of apps that check for drug interactions. Drugs.com, for example, gets over a million queries a month. They’re helpful-but they’re not enough.
Why? Because apps rely on databases that are updated by humans, and they miss about 8% of prescription drugs. Prescription labels? They’re legally required to include every interaction the manufacturer knows about. That’s 100% coverage. Apps also don’t know your exact dose, your kidney function, or whether you’re 78 and on five other meds. Labels are tied to your specific prescription.
Also, apps can’t replace a pharmacist. A 2023 study found that when patients brought all their meds to the pharmacy for a review, potential interactions were caught in 22% of cases. That’s one in five people who thought they were safe-until someone with training looked at the full picture.

What You Need to Do Before You Take Any New Medication
Here’s a simple, step-by-step system that takes less than 3 minutes per medication and cuts your risk of interaction by nearly half:
- Make a full list of everything you take. Not just prescriptions. Include vitamins, supplements, OTC painkillers, herbal teas, and even marijuana or CBD. Write down the dose and how often you take it.
- Bring that list to every doctor and pharmacist visit. Don’t assume they know what you’re on. Only 41% of adults consistently share their full med list. That’s a huge gap.
- When you get a new prescription, ask: "What should I avoid taking with this?" Say it out loud. Don’t wait for them to volunteer it.
- Check the label before you leave the pharmacy. Look for the "Drug Interactions" section. If you don’t see it, ask the pharmacist to point it out.
- Use the Drugs.com checker as a second check-not your first. Enter every item from your list. If it flags something your label doesn’t, bring it up with your provider.
For parents: if you’re giving medicine to a child, use the CDC’s "Check the Label" method: read the label, follow directions, measure with the tool that came with the bottle. Dosing errors are the #1 reason kids end up in the ER for medication issues.
What to Do If You Already Took a Risky Combo
Accidents happen. Maybe you took ibuprofen with your blood thinner and didn’t realize it was risky. Or you started a new supplement and now feel dizzy.
Here’s what to do:
- Stop the new medication. Don’t wait to see if it gets worse.
- Call your pharmacist. They’re trained to handle this. They can tell you if it’s an emergency or if you just need to monitor.
- If you have symptoms like bleeding, chest pain, confusion, or trouble breathing-call 911. Don’t wait. Don’t Google it.
- Update your med list. Add the interaction so you never repeat it.
Don’t feel guilty. Most people don’t know what to look for. The system isn’t perfect. But you can make it work for you.
The Future Is Changing-But Don’t Wait for It
The FDA is updating prescription labels to make them clearer. By late 2025, manufacturers will have to highlight the most critical interactions in bold. They’re also testing QR codes on bottles that link to updated interaction info.
But here’s the truth: you can’t wait for the system to fix itself. Right now, 45 million adults in the U.S. struggle to read health information at a 10th-grade level. Many of them are older, on multiple meds, and at the highest risk. The labels are there. The warnings are written. You just need to know how to read them.
Start today. Grab your next prescription bottle. Find the "Drug Interactions" section. Read it out loud. Ask one question. Write one note. That’s how you stop a hospital visit before it starts.
What should I do if I can’t understand the warnings on my prescription label?
Ask your pharmacist to explain it in plain language. Pharmacists are required to help patients understand their medications. You can also call the toll-free number on the label-most drug manufacturers have a patient support line. Don’t guess. Don’t ignore it. If you don’t understand, you’re at risk.
Are herbal supplements really dangerous with prescription drugs?
Yes, and they’re often overlooked. Supplements like ginkgo biloba, garlic, and St. John’s wort can interfere with blood thinners, antidepressants, and heart medications. Only 17% of prescription labels mention herbal interactions-even though they cause over a third of serious drug reactions. Always list every supplement you take, even if you think it’s "natural" or "safe."
Can I trust the drug interaction checker on my phone app?
Use it as a backup, not your main tool. Apps like Drugs.com are accurate about 89% of the time, but they don’t cover every drug, and they don’t know your personal health details. Your prescription label is legally required to include all known interactions for your exact medication. Always start there.
Why do some labels say "use with caution" instead of "avoid"?
"Use with caution" means the interaction is possible but not guaranteed to be dangerous. Your doctor may still want you to take both drugs, but they’ll need to monitor you closely-like checking your blood pressure or running lab tests. Don’t assume it’s safe just because it’s not "avoid." Pay attention to symptoms and follow up with your provider.
I take five or more medications. How do I keep track of all the interactions?
Keep a written or digital list updated every time you get a new prescription or stop one. Bring it to every appointment. Use a free app like Medisafe or MyTherapy to track doses and alerts. Ask your pharmacist to do a full med review every six months. People on five or more meds are 68% more likely to have an interaction they didn’t catch-so you need to be extra careful.
What if my doctor prescribes something that conflicts with my current meds?
Ask your doctor: "Is there a safer alternative?" or "Can we adjust the dose to make this combination safe?" Don’t assume they know everything on your list unless you told them. Many doctors don’t have time to review every interaction. You’re the best advocate for your own safety. If you’re unsure, get a second opinion from a pharmacist.
Final Tip: Make It a Habit
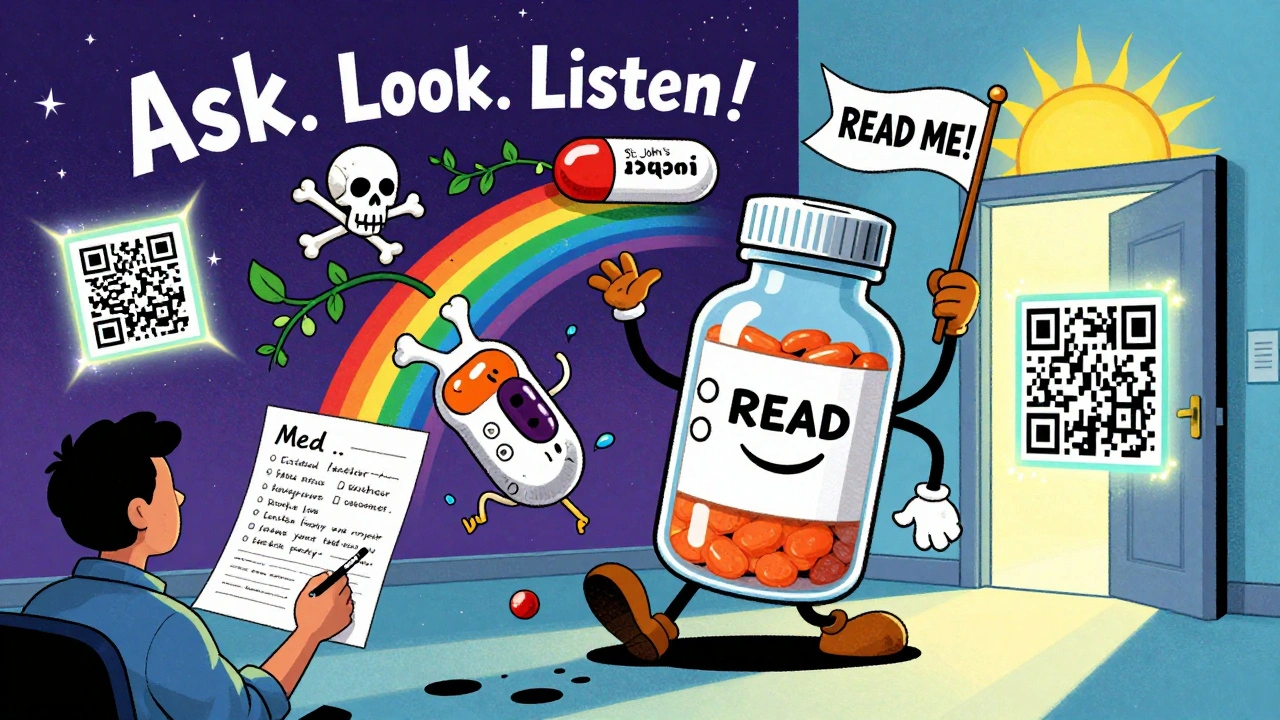
Reading your prescription label isn’t a one-time task. It’s part of taking care of yourself. Every new medication, every refill, every change in your health-those are all moments to double-check. You don’t need to be a doctor. You just need to be curious. Ask. Look. Listen. That’s how you stay safe.
Shofner Lehto
December 5, 2025 AT 01:02I used to skip the label like everyone else until my grandma ended up in the ER because she mixed warfarin with ginkgo. She thought herbal meant safe. Now I read every label out loud before I take anything. It takes 30 seconds. Could save your life.
George Graham
December 6, 2025 AT 05:47This is the kind of post that makes you pause. I work with elderly patients and see this over and over-people think the pharmacist already checked everything. But pharmacists are swamped. You’re the only one who knows your whole list. Writing it down and bringing it to every visit? Non-negotiable.
John Filby
December 6, 2025 AT 21:52Just read my new blood pressure med label and found a warning about grapefruit juice. I didn’t even know that was a thing. I thought it was just a myth. Now I’m double-checking every single thing I take-even my turmeric capsules. Thanks for the nudge. This stuff matters.
Elizabeth Crutchfield
December 8, 2025 AT 21:50omg i just realized i’ve been taking melatonin with my antidepressant and never checked… this post scared me but also saved me. gonna call my pharmacist right now.
Ben Choy
December 9, 2025 AT 10:23Love this. I’m from the UK and we don’t always get the same label clarity, but the principle’s the same. I always ask my pharmacist: ‘What’s the one thing I shouldn’t mix with this?’ They appreciate the question. It makes their job easier too.
Emmanuel Peter
December 10, 2025 AT 16:22Look, most people are lazy. They don’t read labels because they think it’s ‘not their job.’ But here’s the truth: if you’re on more than 3 meds, you’re basically playing Russian roulette with your liver. The system is broken and you’re the only one who cares enough to fix it. Stop waiting for someone else to protect you.
Ashley Elliott
December 12, 2025 AT 08:24One thing I’ve learned after years of managing chronic illness: if a label says ‘use with caution,’ that’s code for ‘this could go sideways, so watch your body like a hawk.’ I keep a little notebook next to my meds. I write down every new symptom-even if it seems small. That’s how I caught my first dangerous interaction.
Chad Handy
December 14, 2025 AT 05:05I’ve been on 11 different prescriptions for my autoimmune stuff, plus 6 supplements, and I swear I’ve read every label five times. But here’s what nobody tells you: the interactions change based on your kidney function, your age, your gut microbiome, even your sleep schedule. The label doesn’t know that. Apps don’t know that. Your doctor might not even know that. So what’s the point? I just stopped taking half the stuff and started eating real food. That’s the real solution.
And don’t get me started on CBD. People think it’s harmless because it’s ‘natural.’ It’s a CYP3A4 inhibitor, which means it can turn your blood thinner into a bomb. I’ve seen three people nearly die because they thought CBD was like chamomile tea. It’s not. It’s a drug. Treat it like one.
And yeah, I know you’re thinking ‘I’m healthy, I don’t need this.’ But you don’t know what you don’t know. And when you end up in the hospital with internal bleeding because you took Advil with your anticoagulant, you won’t be thinking ‘I didn’t read the label.’ You’ll be thinking ‘Why didn’t someone tell me?’
So here’s my advice: stop scrolling. Stop assuming. Open that bottle. Read the tiny print. Even if it’s boring. Even if you’re tired. Even if you think you’re fine. Because one day, you won’t be.
And if you’re reading this and you’re still not doing it? You’re not just risking your life-you’re risking your family’s peace of mind. That’s not hyperbole. That’s the truth.
I’ve been where you are. I’m not trying to scare you. I’m trying to save you.
Joe Lam
December 15, 2025 AT 22:58Wow. This post reads like a public service announcement from 2007. Do you really think people need a 2,000-word essay to understand ‘read the label’? The FDA doesn’t need to ‘update’ anything. People just need to stop being lazy and start reading. Also, apps are 90% accurate-your label is just a legal document written by lawyers who don’t care if you understand it. The real solution? Stop taking so many pills.
Scott van Haastrecht
December 17, 2025 AT 05:09Oh great. Another ‘read your label’ post. Let me guess-you’re one of those people who thinks a pharmacist is your best friend? Newsflash: they’re paid by the pharmacy chain to push generics and upsell vitamins. And your ‘step-by-step system’? It’s a scam. The real reason people have bad reactions is because doctors prescribe like they’re playing Tetris. You’re not the hero here. The system is broken. And you’re just feeding people false hope with bullet points.
Ollie Newland
December 17, 2025 AT 06:10Right, so the CYP3A4 pathway is the key metabolic route for over 50% of clinically used drugs-so when you see ‘inhibitor’ or ‘substrate’ on the label, that’s not jargon, that’s pharmacokinetic reality. But yeah, most folks just glaze over it. The fact that 98% of OTC labels include interaction info but only half read it? That’s not ignorance-it’s systemic health literacy failure. We need mandatory patient education in schools. Not another app. Not another pamphlet. Real curriculum.