Combining Multiple Sedatives: The Hidden Danger of Central Nervous System Depression
 Feb, 2 2026
Feb, 2 2026
CNS Depressant Combination Checker
Check Your Medication Combination
Select all medications you're currently taking. This tool identifies potentially dangerous combinations of central nervous system depressants.
Select medications to check your combination
Use this tool to identify dangerous combinations of central nervous system depressants.
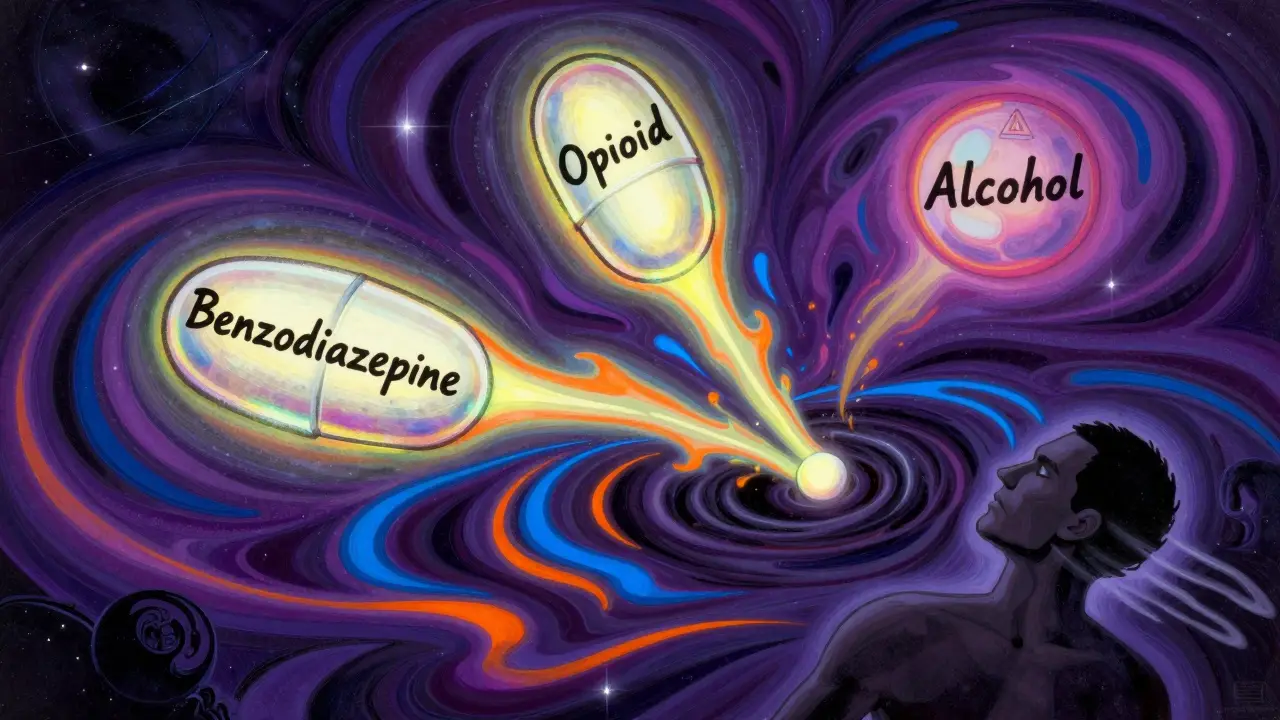
When you take one sedative, your body slows down a little. Take two, and it slows down more. But take three - or mix alcohol with a sleeping pill and a painkiller - and your body doesn’t just slow down. It can stop. This isn’t theoretical. It’s happening right now, in homes, hospitals, and emergency rooms across the UK and beyond. The combination of multiple central nervous system (CNS) depressants is one of the most underreported but deadly drug interactions in modern medicine.
What Happens When Sedatives Team Up?
CNS depressants - including benzodiazepines like diazepam, opioids like oxycodone, barbiturates, sleep meds like zolpidem, and even alcohol - all work the same way: they boost GABA, a brain chemical that tells your nervous system to chill out. Individually, they’re prescribed for anxiety, insomnia, or pain. Together, they don’t just add up. They multiply. This is called synergistic depression - where the combined effect is far worse than the sum of the parts.
Imagine your breathing as a car engine. One sedative might make it idle a little slower. Two might cause it to sputter. Three? It shuts off. Respiratory rate can drop from a normal 12-20 breaths per minute to 4-6. Oxygen levels plunge below 90%, then 85%. Within 15-20 minutes, brain damage can begin. After 4-6 minutes without oxygen, the risk of permanent injury or death rises sharply. The FDA warned in 2016 that combining opioids and benzodiazepines increases the risk of fatal overdose by 2.5 to 4.5 times. That’s not a small risk. That’s a death sentence waiting to happen.
Who’s Most at Risk?
You might think this only happens to people with substance use disorders. It doesn’t. The biggest group at risk? Older adults. Elderly patients are often prescribed multiple medications - one for arthritis, another for sleep, a third for anxiety. They don’t always realize these drugs interact. Studies show that seniors on three or more CNS depressants are 2.8 times more likely to fall and 3.4 times more likely to break a hip. Falls aren’t just injuries - they’re gateways to hospitalization, long-term care, and death.
Women are also at higher risk. Research shows women are 1.7 times more likely than men to be prescribed multiple sedatives. Depression plays a role too - people with depression are over twice as likely to mix these drugs, often unintentionally. And it’s not just pills. Alcohol is the most common hidden ingredient. One in five people on chronic opioid therapy admit to drinking within two hours of taking their painkiller. That’s not a social habit. That’s a medical emergency waiting to unfold.
The Silent Toll: Long-Term Damage
It’s not just about overdoses. Even if you never pass out, mixing sedatives over time quietly wrecks your body. Long-term users report chronic fatigue, weight gain of 12-18 pounds in a year, sexual dysfunction, and worsening depression. One in five develop suicidal thoughts after just six months of combined use. Sleep apnea becomes common - 27% of long-term users develop it. Your brain doesn’t just slow down - it forgets. A major study found that people on multiple CNS depressants had a 27% higher risk of cognitive decline - measurable as a five-point drop on memory tests. That’s not normal aging. That’s drug-induced brain fog.

Common Dangerous Combinations
Some pairings are more lethal than others. Here are the most dangerous combinations you need to know:
- Opioid + Benzodiazepine: The deadliest combo. Responsible for thousands of deaths each year. Even low doses can be fatal.
- Opioid + Alcohol: Alcohol enhances opioid effects, increasing respiratory depression and overdose risk.
- Benzodiazepine + Sleep Medication (e.g., zolpidem): Double sedation. Leads to confusion, amnesia, and dangerous nighttime wandering.
- Barbiturate + Any CNS Depressant: Barbiturates are older, more potent, and less controlled. Mixing them with anything else is extremely risky.
- SSRIs + CNS Depressants: SSRIs can block how your body clears other drugs, causing dangerous buildups. Nearly 70% of depression-related hospitalizations involve multiple CNS drugs.
Why Doctors Still Prescribe These Combos
It’s not that doctors are careless. It’s that the system is broken. Many patients see multiple specialists - a pain doctor, a psychiatrist, a sleep clinic. None talk to each other. Electronic health records rarely flag dangerous interactions unless they’re extreme. A 2020 study found that 10.2% of patients on long-term opioids still received benzodiazepines, despite CDC guidelines against it. Clinicians often have “relatively little guidance” on which combinations are safe - if any.
And patients? They don’t always tell their doctors about over-the-counter sleep aids, herbal supplements, or weekend drinking. They assume if it’s prescribed, it’s safe. Or they’re too embarrassed to admit they’re using alcohol to help them sleep.
What You Can Do
If you’re on any of these drugs - even one - here’s what you need to do:
- Ask your doctor for a full med review. Bring every pill, patch, and bottle - including supplements and alcohol use. Don’t leave anything out.
- Ask: “Is this combination safe?” Specifically name each drug you’re taking. Don’t assume they know what’s in your medicine cabinet.
- Never mix alcohol with sedatives. Not even a glass of wine. Not even once.
- Look for non-drug alternatives. For anxiety: CBT therapy. For insomnia: sleep hygiene, light therapy, or melatonin (with doctor approval). For pain: physical therapy, acupuncture, or mindfulness.
- Ask about deprescribing. Reducing or stopping one sedative can cut your fall risk by 32% and cognitive decline by 27% within a year.
The Future: Safer Systems
Change is coming. The FDA now requires black box warnings on opioid and benzodiazepine labels. The CDC has pushed for reduced co-prescribing - and saw a 15% drop in risky combinations between 2014 and 2018. Hospitals using clinical decision support tools have cut dangerous prescribing by 28%. By 2025, most major EHR systems will auto-flag dangerous combinations before a prescription is even written.
But until then, the responsibility falls on you. No doctor, no app, no warning label can replace your own awareness. If you’re taking more than one sedative, you’re playing Russian roulette with your breathing. It’s not worth the risk.
Can I just take one sedative and one alcohol?
No. Even one sedative plus alcohol can cause dangerous respiratory depression. The combination lowers your breathing rate and impairs your ability to wake up if you stop breathing. There is no safe amount of alcohol when you’re on any CNS depressant.
Are natural sleep aids like melatonin safe to mix with sedatives?
Melatonin itself isn’t a CNS depressant, but it can enhance the sedative effects of other drugs. Taking it with benzodiazepines or opioids can make you overly drowsy, dizzy, or confused. Always check with your doctor before combining any supplement with prescription sedatives.
What should I do if someone I know overdoses on sedatives?
Call 999 immediately. Do not wait. If naloxone is available and the person took an opioid, give it. But naloxone won’t reverse benzodiazepine or alcohol overdose. Keep the person awake and on their side until help arrives. Never leave them alone.
Can I stop taking my sedatives cold turkey?
No. Stopping suddenly, especially after long-term use, can cause seizures, hallucinations, or life-threatening withdrawal. Always work with your doctor to taper off safely. A gradual reduction over weeks or months is the only safe approach.
Are there any sedatives that are safe to combine?
There are no officially approved combinations of multiple CNS depressants. Even drugs that seem mild - like antihistamines or muscle relaxants - can add to the risk. The safest choice is to use only one sedative at a time, if absolutely necessary, and never mix with alcohol or other depressants.
Final Thought
Sedatives aren’t harmless. They’re powerful drugs that affect your most basic life functions - breathing, heart rate, consciousness. Combining them isn’t a shortcut to feeling better. It’s a path to irreversible harm. If you’re taking more than one, talk to your doctor today. Your life depends on it.
Amit Jain
February 3, 2026 AT 05:21Been working in rural India with elderly patients for 10 years. Saw this happen too many times - grandpa takes pain pills, grandma gives him sleep tea, and they both drink chai with alcohol. No one tells the doctor. Simple fix: talk to them. Use pictures, not big words. They understand.
One man stopped mixing after his grandson showed him a video. He said, 'I didn’t know my breathing was stopping.' Now he walks daily. Life changed.
Don’t overcomplicate it. Just ask. Listen. Care.
Geri Rogers
February 3, 2026 AT 12:15THIS. SO. MUCH. 🙏 I’m a nurse and I’ve seen too many old folks code because they took Xanax for anxiety, oxycodone for back pain, and ‘just one glass of wine’ to relax. ONE GLASS. THAT’S ALL THEY SAID. Then they woke up in ICU with a breathing tube.
Doctors don’t ask. Patients don’t tell. System’s broken. But YOU can fix it - ask your grandma what meds she’s taking. Don’t assume. Don’t wait. Save a life today. 💪❤️
Janice Williams
February 3, 2026 AT 16:00One must question the fundamental premise of this article: that individual autonomy in pharmaceutical consumption should be subjugated to institutional oversight. The notion that adults cannot responsibly manage their own CNS depressant intake is both patronizing and statistically unfounded. The FDA’s warnings, while well-intentioned, reflect a broader cultural trend of infantilization under the guise of public health.
Moreover, the conflation of recreational alcohol use with clinical sedative misuse is a deliberate rhetorical tactic to induce fear, not inform. One may consume a single glass of wine with a low-dose benzodiazepine without consequence - provided one is not an alcoholic, a child, or a morbidly obese individual. Context matters. And context, it seems, is now considered dangerous.
Ed Mackey
February 3, 2026 AT 17:47My uncle died from this. Took his pain med, had a beer, fell asleep in his chair. We found him 8 hours later. No one knew he was on three meds. The ER doc said it was 'a perfect storm.'
But here’s the thing - he didn’t even know he was mixing. His docs never talked. His sister gave him melatonin 'for sleep.' His buddy told him 'a little whiskey helps the pills go down.'
Just... talk to your family. Seriously. Even if it’s awkward. It’s worth it.
Katherine Urbahn
February 5, 2026 AT 16:38It is, indeed, a matter of grave concern that the medical establishment continues to permit, and even facilitate, the concurrent prescription of multiple central nervous system depressants. The data presented herein is not merely suggestive-it is unequivocal. Moreover, the failure of electronic health records to consistently flag these interactions constitutes a systemic dereliction of duty. One cannot, in good conscience, permit such negligence to persist under the banner of 'clinical autonomy.'
Furthermore, the normalization of alcohol consumption in conjunction with prescribed sedatives is not merely irresponsible-it is a public health catastrophe, perpetuated by cultural complacency and professional apathy. The responsibility lies not solely with patients, but with institutions that have abdicated their duty to safeguard life.
Joseph Cooksey
February 6, 2026 AT 22:07Let’s be real here - this isn’t just about pills and alcohol. It’s about loneliness. It’s about sleepless nights with aching joints and a mind that won’t shut off. It’s about being told, 'Here, take this,' by five different doctors who never sit in the same room together. It’s about a 72-year-old woman who drinks because she’s terrified of the silence after her husband died. She doesn’t want to 'mix' - she just wants to feel human again.
So yeah, the combo is deadly. But the real danger? The system that gives her three prescriptions and then calls her reckless when she uses them together. We’re not talking about drug addicts here. We’re talking about people who’ve been failed by medicine, by family, by society. And now we’re blaming them for surviving?
Fix the system before you fix the patient. Otherwise, you’re just putting band-aids on a hemorrhage.
Coy Huffman
February 8, 2026 AT 16:09Been thinking about this a lot lately. I used to take zolpidem for sleep, then added a low-dose benzo for anxiety. Thought I was being careful. Turns out, I was just slowly shutting down.
Had a panic attack last month - couldn’t breathe. Thought I was dying. Turned out I was just overdosing on sleep. No alcohol. Just meds. Scared the hell out of me.
Now I’m doing CBT, walking every morning, and only taking one thing at night - and even then, only when I really need it. My brain feels clearer. I’m not 'addicted' - I’m just awake again.
It’s not about willpower. It’s about awareness. And yeah, I’m still learning.
Harriot Rockey
February 9, 2026 AT 15:48My mom’s on three of these. I just started asking her every Sunday: 'What did you take this week?' No judgment. Just love. She cried and said no one ever asked before. We made a list. We called her pharmacist. She’s cutting back one med at a time.
It’s not perfect. But she’s sleeping better. And she’s not falling anymore.
❤️ You’re not alone. Talk to someone. Even just one person.
rahulkumar maurya
February 9, 2026 AT 20:32It is amusing how Western societies have elevated pharmacological convenience to the status of moral imperative. The very notion that one must 'deprescribe' implies a failure of personal discipline. One is not a victim of polypharmacy - one is a victim of weak will and poor intellectual fortitude.
Moreover, the assertion that 'no safe combination exists' is a gross oversimplification. The human body is not a spreadsheet. It is a complex, adaptive system. To reduce it to a list of 'dangerous pairings' is the hallmark of a society that fears nuance.
And yet - the real tragedy is not the drug interaction. It is the surrender of autonomy to institutional dogma.
Demetria Morris
February 9, 2026 AT 21:49I used to take Ambien and Klonopin together. I didn’t think it was a big deal. I was depressed. I thought I deserved to sleep. Then I woke up on the floor, bleeding from my head, with no memory of how I got there.
I didn’t drink. I didn’t do drugs. I just trusted my doctors. They didn’t warn me. I didn’t know to ask.
I’m not mad. I’m just… done pretending it’s okay. I’m tapering. Slowly. With help.
Don’t wait until you wake up broken.
Susheel Sharma
February 10, 2026 AT 01:27Let’s be honest - this article is just another fear-mongering op-ed dressed up as public health. The real issue? Overprescribing by overworked doctors who don’t have time to think. But the solution isn’t to shame patients - it’s to fix the system. Why are we letting primary care physicians manage psychiatric meds? Why are neurologists prescribing sleep aids?
And let’s not pretend alcohol is the villain. It’s a cultural artifact. The real problem is the commodification of mental health. We treat anxiety like a broken lightbulb. You replace it. Done.
Meanwhile, the people who actually suffer are left to figure it out alone.
Also, melatonin is fine. Chill out.
Roshan Gudhe
February 10, 2026 AT 05:05There’s a quiet kind of suffering here. Not the screaming overdose kind. The slow fade. The forgetting where you put your keys. The days that blur together because you’re always half-asleep.
I used to think I was just getting older. Turns out, I was just drugged up.
My doctor didn’t know I was taking two sleep aids. I didn’t know they were both depressants. I thought melatonin was 'natural' so it was safe.
Turns out, 'natural' doesn’t mean 'harmless.'
Now I walk at dawn. I read. I sit in silence. I’m still tired. But I’m me again.
It’s not about quitting. It’s about remembering who you are before the pills.
Rachel Kipps
February 10, 2026 AT 15:20I’m a geriatric nurse. I’ve seen this so many times. One patient took her pain pill, her anxiety med, and her 'herbal sleep aid' - which turned out to be kava root. She stopped breathing. We revived her.
She didn’t know kava was a depressant. No one told her.
Doctors assume patients know. Patients assume doctors know.
It’s a silent gap. And people are dying in it.
Just… ask. Even if it’s awkward.
Wendy Lamb
February 11, 2026 AT 18:08One med. One time. No alcohol. Period.
That’s it.
Antwonette Robinson
February 13, 2026 AT 17:03Oh wow, a 12-page essay on how not to die from being tired. Did you also include a flowchart for when to call 911? Maybe a PowerPoint on why 'just one glass' is a lie?
Wow. Groundbreaking. Next up: 'Warning: Breathing Can Be Dangerous If Done Too Much.'
Also, I take melatonin and wine. I’m fine. Thanks for the scare tactic.