Understanding DPP-4 Inhibitors: How Sitagliptin Lowers Blood Sugar
 Jul, 13 2025
Jul, 13 2025
Picture this. You wake up, grab your favorite morning coffee, maybe nibble on a piece of fruit, and head off to work. Your blood sugar hums quietly in the background, regulated by a tiny orchestra of hormones and enzymes. But for people with Type 2 diabetes, this system’s harmony is easily disrupted. Here’s the kicker: a whole class of medications—DPP-4 inhibitors—has changed the way people approach blood sugar control. It’s not your typical medicine that bullies the pancreas to squeeze out more insulin. DPP-4 inhibitors function with a subtlety that’s honestly fascinating. If you’re wondering how these drugs, especially sitagliptin (the well-known Januvia), tackle high blood sugar, you’re in the right place. We’re slicing into the mechanism, the practical facts, and the real-world details you actually want to know.
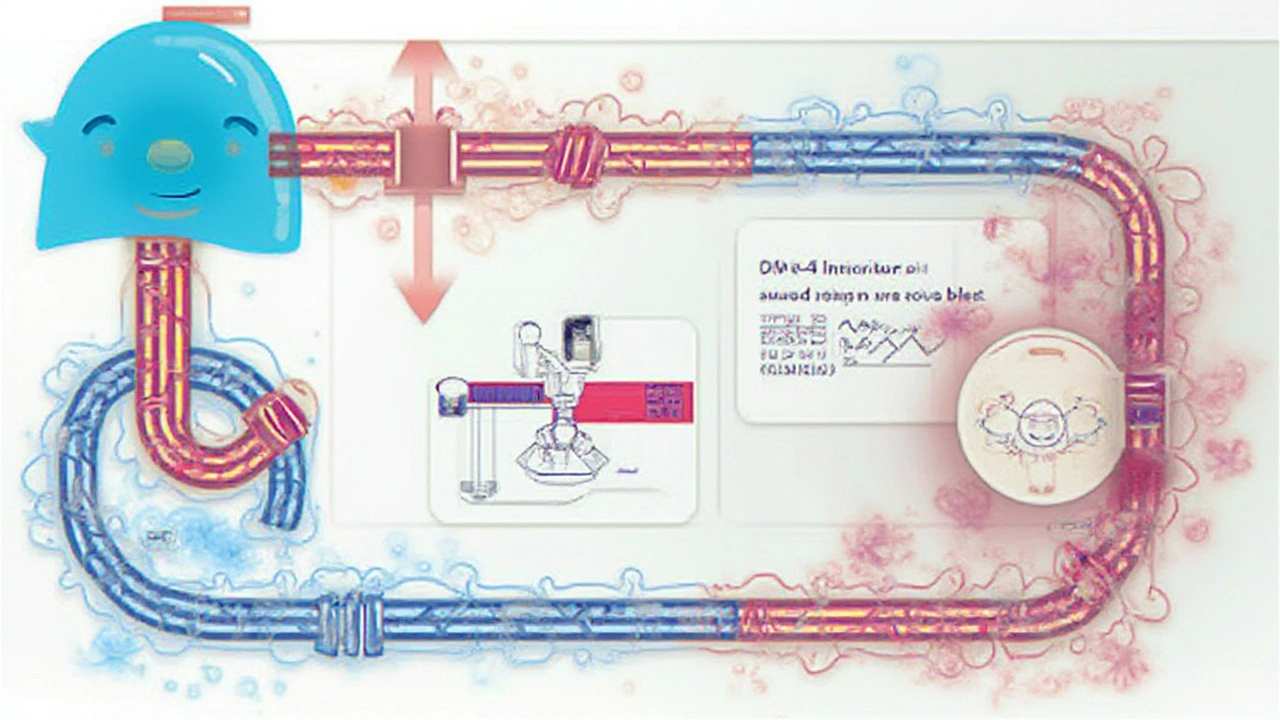
Inside the Science: How DPP-4 Inhibitors Work
It’s wild to think about just how many players get involved every time you eat. The body doesn’t simply churn out insulin and call it a day—there’s this relay race of hormones, and one of the stars is something called incretins. You’ve probably never heard of them unless you’ve hung out at an endocrinology conference, but they basically boost how much insulin your body releases after meals. Problem is, an enzyme named DPP-4 slices and dices those incretins before they get to finish the job. Enter DPP-4 inhibitors. These medicines, with sitagliptin leading the pack, put a roadblock in front of DPP-4. End result: your incretins last longer, so your insulin response is better timed and more robust at the exact moment it’s needed most. And your glucose? More likely to stay within a healthy range.
Let’s get specific. Sitagliptin, saxagliptin, linagliptin, and alogliptin are the big names in this class. They don’t cause the dramatic drops in blood sugar that you see with some older medications. In fact, the risk of hypoglycemia (that scary low blood sugar crash) is super low unless you’re combining them with other diabetes meds that might push sugar down too far. That’s a game-changer for day-to-day living. People don’t want their medication fixing one problem but causing a new headache.
So why the fuss? Clinical studies show sitagliptin and its cousins lower HbA1c by about 0.5–0.8%. That might not sound fireworks-worthy, but paired with their low side effect profile, it makes them an easy add-on when diet, exercise, or metformin alone aren’t cutting it. Plus, you don’t see much weight gain (a huge plus when every pound matters with diabetes care), and there’s barely a blip on the risk-of-heart-trouble radar, according to long-term trials.
If you like numbers, here’s a quick table to put the differences in perspective:
| Drug | Avg. HbA1c Reduction (%) | Weight Impact | Hypoglycemia Risk | Standard Dose |
|---|---|---|---|---|
| Sitagliptin | 0.7 | Neutral | Low | 100mg daily |
| Saxagliptin | 0.7 | Neutral | Low | 5mg daily |
| Linagliptin | 0.7 | Neutral | Low | 5mg daily |
| Alogliptin | 0.7-0.8 | Neutral | Low | 25mg daily |
This isn’t old-school medicine; it’s precision tune-up with minimal drama. No wonder DPP-4 inhibitors, especially sitagliptin, remain staples in diabetes care toolkits everywhere.
Who Can Benefit—and When?
Here’s where the story gets real. Who should even think about using a DPP-4 inhibitor like sitagliptin? Doctors usually look at this option for adults with type 2 diabetes who still have some baseline blood sugar control, but not enough to keep things healthy with just diet, exercise, or their first-line medication (most often metformin). If someone can’t tolerate metformin (hello, nausea), sitagliptin often gets bumped up the list.
If you’re the type who hates juggling pills, DPP-4 inhibitors are once-daily. Most people take their dose in the morning, but the timing isn’t super strict. You don’t have to eat with it—convenience matters, right? Sitagliptin, as the pioneer, is especially popular. You’ll find it under the brand name Januvia and as a generic.
People with kidney concerns often do better with sitagliptin than other meds. The dose adjusts depending on how well your kidneys are doing—your doctor runs a blood test (eGFR) every so often to keep an eye on this. No wild guesswork. For those with serious kidney trouble, the dosage can drop by half or even more, all to avoid risking side effects or buildup of medicine in the body.
Now, kids and teenagers with type 2 diabetes are a special case. These drugs aren’t typically the first pick for them, and insurance isn’t always on board, so use is mostly for adults. And FYI—pregnant women or those breastfeeding should avoid DPP-4 inhibitors since safety isn’t clear enough yet.
Ever wonder about using these meds with others? You can definitely layer them with metformin. Pairing with sulfonylureas works, but that’s when the risk of low blood sugar starts to creep higher. Some people even take DPP-4 inhibitors along with insulin, though it’s not the first combo a doctor reaches for. Remember, it’s not about smashing blood sugar down at all costs—it’s about fine-tuning and staying steady day after day.
Let’s talk about insurance and access, because those count just as much. Good news: most major plans cover at least one generic DPP-4 inhibitor, and as generics become more common, out-of-pocket costs are dropping. Januvia’s patent already expired, making the pharmacy bill a lot less painful for many.
Dosing Tips and Monitoring: Getting It Right
All right, dosing isn’t a snooze-fest if you care about living your life on your terms. Basic dosing is straightforward: one pill, once a day. For sitagliptin, that’s usually 100mg—unless your kidneys need a little extra attention, then your doctor might cut it down to 50mg or even 25mg daily. Saxagliptin, linagliptin, and alogliptin each have their own magic numbers, but the rhythm is still the same: just one daily dose.
Here’s a tip from the trenches: set a reminder on your phone so you don’t miss doses. These medications have a long enough action window that missing one pill won’t instantly mess up your glucose, but regularity makes a difference for long-term results.
Your diabetes plan should include blood tests. Regular HbA1c checks show the big picture for glucose. Your doctor looks for a drop of around 0.7%, give or take. Urine and blood tests for kidney function are key before changing doses or if you’re ill. No playing doctor on your own—if you’re unsure, just ask or message your care team.
Don’t be fooled by the low risk of hypoglycemia. If you’re taking other meds that can lower blood sugar (like sulfonylureas or insulin), you might still need to recognize the warning signs—shakiness, sweating, confusion, or sudden hunger. Keep a snack handy just in case. Most people though? No crashes, no drama.
Here’s something direct: Never double your dose if you miss a pill. If you’re unsure, take it as soon as you remember, but skip if it’s almost time for the next dose. Overdoing it doesn’t make your blood sugar better—it just risks side effects.
Want more on the nitty-gritty of how does Januvia work? That link digs into both the mechanism and side effects, super helpful if you’re considering or already using sitagliptin.
If you wind up needing surgery, get sick, or notice swelling, rashes, or signs of pancreatitis (like sudden, intense upper belly pain), it’s best to call your doc pronto. It’s rare, sure, but no need to roll the dice with your health.
Pro-tip: always tell your doctor, dentist, or pharmacist about every med, vitamin, or supplement you take. Interactions are rare but can sneak up when you least expect it, especially if you’re prescribed antibiotics or meds for heart rhythm, seizures, or HIV.
Common Myths, Side Effects, and What to Watch For
It’s easy to get swept up by rumors or YouTube testimonials, but DPP-4 inhibitors aren’t miracle pills or big bad wolves. Some people expect weight loss—these drugs don’t help with dropping pounds. They also don’t cure diabetes, but they absolutely help manage it with less stress about ups and downs.
The most common side effects? Think stuffy nose, mild sore throat, maybe headaches. Sometimes people get tummy aches or diarrhea, especially at the start. Most of those fade out or never show up at all. Serious reactions—like allergic rashes, joint pain, or pancreatitis—are rare, but possible. About one in a thousand experience enough trouble to stop the drug. That’s why open conversations with your provider make a real difference. If anything feels off, trust your gut and get checked out.
Another big question: Do DPP-4 inhibitors affect the heart? Tons of research, including massive studies called TECOS for sitagliptin, found that these drugs don’t boost your risk of heart attack or stroke. There was talk for a while about a slight uptick in heart failure for saxagliptin, but guidelines now suggest doctors use extra caution for patients with heart failure history. For most people though, the data’s reassuring—no massive red flags popping up.
What’s extra cool: these meds don’t mess with your day-to-day. You can travel, eat out, work crazy shifts, and they’re still doing their job quietly in the background. You don’t need to stagger your meal times or overhaul your schedule because of your medication window.
- Don’t split or crush these tablets. The coating helps deliver the dose steadily—you mess that up, you risk an uneven effect.
- Store them at room temperature, away from heavy moisture or light. Bathroom cabinets are out; think bedroom or kitchen, away from the stove.
- Expired pills? Toss them, don’t take the gamble. Your pharmacist will remind you, but it’s worth saying twice.
Getting the best from a DPP-4 inhibitor means pairing it with healthy basics: regular checkups, moving your body (even a 20-minute walk), going easy on the sweets, and keeping up with routine bloodwork. For loads of people, the switch to sitagliptin or its cousins is the difference between feeling stressed out every meal and living a bit more freely.
Emily Nesbit
July 24, 2025 AT 15:08Sitagliptin’s mechanism is elegantly precise-DPP-4 inhibition extends GLP-1 and GIP half-life, enhancing glucose-dependent insulin secretion without stimulating beta-cells directly. This pharmacodynamic profile minimizes hypoglycemia risk compared to sulfonylureas. The HbA1c reduction of 0.7% is statistically significant in meta-analyses, though clinically modest. Weight neutrality is a key advantage in a population where obesity exacerbates insulin resistance. No meaningful cardiovascular risk signal in TECOS trial, which is reassuring. Dosing adjustments for renal impairment are well-characterized, with eGFR thresholds clearly defined in prescribing guidelines. The lack of drug-food interactions simplifies adherence. Still, long-term data beyond 5 years remains limited, and real-world adherence often declines after 12 months due to perceived lack of immediate effect. Not a cure, not a miracle, but a rational, evidence-based adjunct.
John Power
July 24, 2025 AT 20:54Love this breakdown. Seriously, DPP-4 inhibitors are the quiet heroes of diabetes care. I’ve seen patients go from panic attacks before meals to actually enjoying dinner for the first time in years. No crashes, no constant snacking, no guilt. It’s not flashy, but that’s the point-it lets people live. And yeah, the weight neutrality? Huge. So many meds make you gain, and that’s just another burden. If you’re on metformin and still struggling, this is the next logical step. No drama. Just steady control. 🙌
Richard Elias
July 24, 2025 AT 23:02why do ppl keep actin like this drug is magic? its just a bandaid. you still gotta watch what u eat. and the price? still too high even as generic. and dont get me started on how some docs push it like its the new best thing. its not. its just less side effects than metformin for some. thats it. stop hyping it up.
Scott McKenzie
July 25, 2025 AT 17:09Just wanted to add a real-world note: I’ve been on sitagliptin for 3 years. My A1c dropped from 7.8 to 6.4. No weight gain. No lows. I take it with my coffee every morning-no fuss. My doc says my kidneys are fine, so I stay on 100mg. The only side effect? A slightly stuffy nose the first month. Gone now. If you’re on the fence, give it a real shot. It’s not going to fix everything, but it takes the edge off. 🌞
Jeremy Mattocks
July 27, 2025 AT 15:55Let’s not overlook the psychological impact here. For many people with type 2 diabetes, the fear of hypoglycemia is paralyzing-panic attacks before driving, nightmares about passing out at work, avoiding social events because of food anxiety. DPP-4 inhibitors like sitagliptin don’t just lower glucose numbers-they lower emotional burden. The fact that you can eat a slice of pizza without needing to calculate insulin ratios or carry glucose tabs is transformative. It’s not about the 0.7% HbA1c drop on paper-it’s about reclaiming autonomy. You can travel, go out to dinner, sleep through the night without checking your meter. That’s not just pharmacology, that’s quality of life. And yes, it’s not perfect, but when you compare it to the alternatives-injectables, frequent fingersticks, nausea from metformin, weight gain from sulfonylureas-it’s a no-brainer for many. The real win? It’s a pill you can take without feeling like you’re being punished for having diabetes.
Paul Baker
July 27, 2025 AT 17:14so i been on this for 2 years and it works fine but i think the real secret is just walking after dinner 😎 maybe the drug just helps you feel good enough to move more? 🤔
Zack Harmon
July 28, 2025 AT 00:47THIS IS WHY AMERICA IS FALLING APART. PEOPLE ARE TAKING PILLs INSTEAD OF CHANGING THEIR LIVES. YOU WANT TO FIX DIABETES? STOP EATING SUGAR. STOP BEING LAZY. THIS DRUG IS JUST A COP OUT FOR PEOPLE WHO DONT WANT TO TAKE RESPONSIBILITY. THEY’RE GIVING OUT PILLs LIKE CANDY AND NOW KIDS ARE GETTING DIABETES AT 12. THIS ISN’T MEDICINE-IT’S GIVING UP.
Jeremy S.
July 28, 2025 AT 20:32It’s not magic, but it’s not a cop-out either. Works for some. Not for all. No need to hate on it.
Jill Ann Hays
July 28, 2025 AT 23:21The notion that DPP-4 inhibition constitutes therapeutic sophistication is a misapprehension rooted in pharmaceutical marketing narratives. The pharmacokinetic profile is undeniably elegant, yet the clinical utility remains marginal when juxtaposed against the foundational imperative of lifestyle modification. One cannot obfuscate the etiological centrality of caloric excess and sedentary behavior under the veneer of enzymatic modulation. The data, while statistically significant, lacks clinical transformative power. This is palliative pharmacology, not curative intervention. The cultural glorification of pharmacological convenience over behavioral accountability is a symptom of a broader pathological disengagement from physiological responsibility.
Mike Rothschild
July 30, 2025 AT 07:37Good post. I’ve been helping people manage diabetes for over 15 years. Sitagliptin isn’t the answer for everyone but it’s one of the safest tools we have. Especially for older folks or those with kidney issues. I always tell my patients: it’s not about finding the perfect drug. It’s about finding the right fit. And for a lot of people, this is it. Consistency matters more than the pill itself. Take it. Move. Check your numbers. Talk to your doc. That’s the real recipe.
Ron Prince
July 31, 2025 AT 09:29another one of them fancy foreign drugs that cost a fortune. why cant we just use good old insulin like in the old days? this country is so soft now. you take a pill for everything. back in my day we just ate less and walked more. now everyone wants a magic bullet. this is why america is weak.
Sarah McCabe
July 31, 2025 AT 21:43Love how you explained the incretin thing 😊 I’m from Ireland and we’ve got a lot of people on this here too. My uncle’s been on it for 4 years and he says he finally feels like he can have a pint with his mates without worrying. That’s the win right there 🍀