How Cardiac Biomarkers Aid Diagnosis and Management of Hypertrophic Subaortic Stenosis
 Sep, 28 2025
Sep, 28 2025
When evaluating heart disease, cardiac biomarkers are proteins or peptides released into the bloodstream that reflect myocardial injury, stress, or remodeling. Their levels often rise before symptoms become obvious, making them a useful early warning system for clinicians. In the context of Hypertrophic Subaortic Stenosis (HSS) - a form of hypertrophic obstructive cardiomyopathy that blocks blood flow out of the left ventricle - biomarkers help fine‑tune diagnosis, risk stratification and therapy choices.
Why Hypertrophic Subaortic Stenosis Needs More Than an Echo
HSS is characterized by asymmetric septal hypertrophy, a narrowed left ventricular outflow tract (LVOT), and dynamic obstruction that can vary with heart rate or volume status. While echocardiography remains the gold standard for measuring wall thickness and LVOT gradient, it doesn’t capture the biochemical stress the heart endures. That’s where cardiac biomarkers step in - they provide a window into the cellular level of injury and can alert clinicians to hidden decompensation.
Key Biomarkers and What They Tell Us
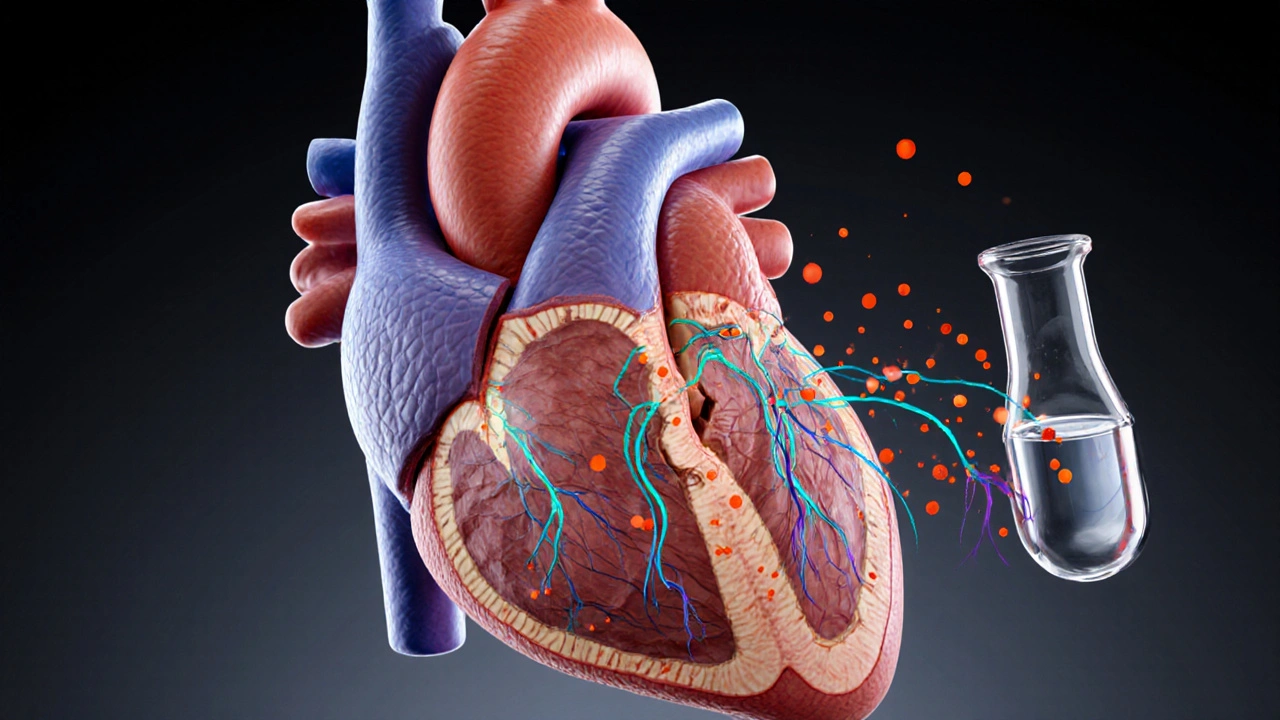
- Troponin I - the most specific marker for myocardial necrosis. Even modest elevations in HSS often signal micro‑infarction caused by high LVOT pressures.
- B‑type Natriuretic Peptide (BNP) - released when ventricular walls stretch. In HSS, BNP correlates tightly with symptom severity and LVOT gradient.
- NT‑proBNP - the inactive N‑terminal fragment of BNP. It has a longer half‑life, making it useful for monitoring chronic pressure overload.
- Creatine Kinase‑MB (CK‑MB) - rises in acute injury but is less specific than troponin. Still, in HSS patients undergoing stress testing, CK‑MB provides extra context.
- High‑sensitivity Troponin T (hs‑cTnT) - detects tiny leaks of cardiac protein, helpful for early risk stratification.
When to Order Which Test
- Baseline assessment: At initial diagnosis, draw troponin I, BNP, and NT‑proBNP to establish a biochemical floor.
- Symptom flare‑up: If a patient reports new dyspnea or chest discomfort, repeat troponin I and CK‑MB to rule out ischemia triggered by obstruction.
- Pre‑procedure screening: Before septal myectomy or alcohol septal ablation, obtain hs‑cTnT and NT‑proBNP to gauge peri‑operative risk.
- Long‑term monitoring: Quarterly BNP or NT‑proBNP measurements track how well medical therapy (beta‑blockers, disopyramide) is unloading the ventricle.
How Biomarkers Influence Management Decisions
Elevated troponin in a “stable” HSS patient often nudges the heart team toward more aggressive therapy - either higher‑dose beta‑blockade or earlier referral for invasive septal reduction. Conversely, a normal BNP despite a high LVOT gradient may suggest that the patient’s heart is tolerating the obstruction, allowing a watch‑and‑wait approach.
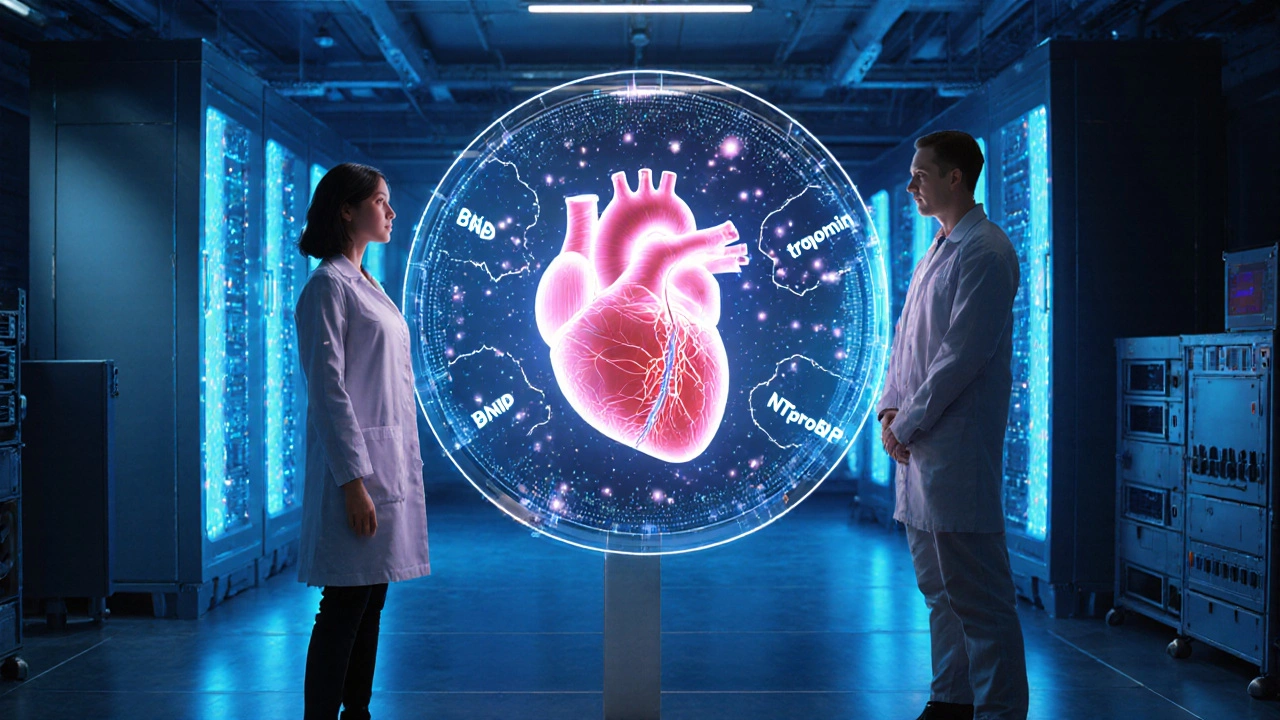
Risk scores such as the European Society of Cardiology’s HCM‑Risk model now integrate NT‑proBNP values to predict sudden cardiac death (SCD). Patients with NT‑proBNP > 1000pg/mL routinely qualify for an implantable cardioverter‑defibrillator (ICD) discussion, especially if they also carry high‑risk genetic mutations.
Genetic Context: Linking Biomarkers to Underlying Mutations
Approximately 60% of HSS cases trace back to sarcomere gene variants - most commonly MYH7 and MYBPC3. Studies published in 2024 show that MYH7 carriers often present with higher troponin peaks during exertion, while MYBPC3 carriers display more pronounced BNP elevations at rest. Knowing a patient’s genotype helps clinicians interpret biomarker trends more accurately.
Limitations and Pitfalls
Biomarker levels can be confounded by renal insufficiency, pulmonary hypertension, or even intense physical training. In older adults, baseline BNP may be chronically elevated, diluting its diagnostic value. Moreover, assay variability between laboratories sometimes leads to misleading serial comparisons. Always interpret results alongside imaging and clinical context.
Future Directions: Emerging Markers
Researchers are investigating galectin‑3 and ST2 as fibrosis markers that could predict progression from non‑obstructive hypertrophy to full‑blown HSS. Early trials suggest that rising galectin‑3 levels precede symptom onset by up to two years, offering a potential window for preventive therapy.
Another promising avenue is multi‑omics panels that combine proteomics, metabolomics, and microRNA signatures. When integrated with AI‑driven risk models, these panels may someday replace the need for repeated echocardiograms in low‑risk patients.
| Biomarker | Primary Signal | Typical Elevation Threshold | Clinical Use |
|---|---|---|---|
| Troponin I | Myocyte necrosis | >0.04ng/mL | Detect micro‑infarction during obstruction spikes |
| BNP | Ventricular wall stretch | >100pg/mL | Gauge symptom severity, monitor therapy response |
| NT‑proBNP | Long‑term stretch | >300pg/mL | Risk stratification for SCD, long‑term follow‑up |
| CK‑MB | Acute injury | >5µg/L | Adjunct in stress‑test related chest pain |
| hs‑cTnT | Very low‑level leakage | >14ng/L | Early risk assessment, especially in young athletes |
Practical Checklist for Clinicians
- Obtain baseline troponin I, BNP, NT‑proBNP at diagnosis.
- Repeat biomarkers when symptoms change or before any invasive procedure.
- Interpret BNP/NT‑proBNP in the context of renal function and age.
- Integrate genetic testing results (e.g., MYH7, MYBPC3) to refine biomarker thresholds.
- Use elevated NT‑proBNP (>1000pg/mL) as a trigger for ICD discussion.
- Stay aware of emerging markers like galectin‑3 - they may become part of routine panels within the next few years.
Frequently Asked Questions
Can a normal troponin rule out serious obstruction in HSS?
No. Troponin mainly signals cell death. A patient can have a high LVOT gradient with normal troponin if the myocardium is still coping. Combine the result with BNP levels and echo findings for a full picture.
How often should BNP be measured in a stable HSS patient?
Every 3‑6months is common practice, especially when medication doses are adjusted. More frequent checks are warranted after any symptom escalation or procedural intervention.
Do genetic mutations affect biomarker thresholds?
Evidence suggests MYH7 carriers may show higher troponin spikes during exertion, while MYBPC3 carriers tend to have higher resting BNP. Tailoring thresholds to genotype improves risk prediction.
Is NT‑proBNP better than BNP for long‑term monitoring?
Generally yes. NT‑proBNP has a longer half‑life and is less affected by acute fluctuations, making it more reliable for tracking chronic pressure overload.
What emerging biomarker looks most promising for HSS?
Galectin‑3, a marker of cardiac fibrosis, has shown a strong correlation with disease progression in early trials. It may soon complement BNP in risk models.
In short, cardiac biomarkers aren’t a stand‑alone diagnosis tool for hypertrophic subaortic stenosis, but they are a powerful adjunct that shines a light on myocardial stress, guide therapeutic decisions, and flag patients who need closer surveillance.
Tionne Myles-Smith
September 29, 2025 AT 05:44This is such a clear, practical breakdown-I’ve seen so many residents overlook biomarkers and just rely on echo alone. Seriously, BNP and NT-proBNP should be part of every HSS baseline panel. I’ve had patients with normal gradients but sky-high BNP who turned out to be on the verge of decompensation. It’s wild how much these little proteins tell us.
Also, the genetic link part? Mind blown. MyH7 vs MYBPC3 differences make total sense now-I’ll be adjusting my interpretation game from now on.
Jordyn Holland
September 29, 2025 AT 15:50Of course you’re all acting like this is groundbreaking. Everyone who’s been in cardiology for more than two years already knows this. And yet, here we are-2024-and still seeing clinicians treat HSS like it’s 2010. The fact that you need a whole article to explain that BNP correlates with LVOT gradient is… almost embarrassing.
Also, ‘galectin-3’? Really? That’s your ‘promising’ marker? We’ve had that data since 2018. You’re late to the party, and you brought snacks.
And why are we still using CK-MB? It’s obsolete. Like using a rotary phone in a 5G world.
Jasper Arboladura
September 29, 2025 AT 17:46The article is technically accurate but lacks nuance in the clinical application. The thresholds cited are lab-specific and not universally applicable. For instance, the 100 pg/mL BNP cutoff assumes normal renal function and absence of atrial fibrillation-both of which are frequently violated in real-world practice.
Furthermore, the assertion that NT-proBNP >1000 pg/mL automatically triggers ICD discussion ignores the ESC HCM-Risk-SCD model’s multivariate nature. Relying on a single biomarker threshold is dangerously reductive. Also, the genetic correlation data is preliminary-most studies are single-center with small cohorts. Correlation ≠ causation.
And please, stop calling it ‘HSS.’ It’s HCM with LVOTO. Terminology matters.
Joanne Beriña
October 1, 2025 AT 02:38Why are we letting foreign labs dictate our biomarker thresholds? The US has the best cardiac labs in the world-why are we using European cutoffs? This is why our healthcare system is broken. We need American-made biomarkers with American standards!
Also, why is everyone ignoring the fact that these markers are being used to justify invasive procedures that cost $50k? We’re turning healthy people into patients with labels. This is profit-driven medicine, not science.
And what about natural remedies? I’ve seen patients reverse HSS with turmeric and breathwork. Why isn’t that in the article? Because Big Pharma owns this narrative.
ABHISHEK NAHARIA
October 1, 2025 AT 12:42While the biochemical framework presented is methodologically sound, one must question the epistemological hierarchy of biomarkers over clinical phenomenology. In Indian cardiology practice, where echocardiographic access remains uneven, reliance on serum markers may exacerbate diagnostic inequity.
Furthermore, the Western-centric thresholds for NT-proBNP do not account for ethnic variations in cardiac physiology. South Asian populations exhibit higher baseline BNP even in the absence of structural heart disease, rendering these cutoffs potentially misleading in our context.
One wonders whether this is medicine or data colonialism dressed as innovation.
Hardik Malhan
October 2, 2025 AT 18:01BNP and NT-proBNP are not interchangeable. Half-life difference is key. NT-proBNP is more stable but less responsive to acute changes. Use NT for longitudinal tracking, BNP for acute events.
hs-cTnT >14 ng/L in young athletes with septal hypertrophy = red flag for microinfarction even without symptoms. Don’t wait for troponin to spike. Start beta-blockers early.
Genotype matters. MYH7 = higher troponin spikes under stress. MYBPC3 = chronic BNP elevation. Adjust interpretation accordingly.
Renal function > biomarker value. Always.
Casey Nicole
October 2, 2025 AT 20:25Let’s be real-this whole biomarker obsession is just another way to monetize heart disease. Every time someone gets a blood test, someone gets paid. Meanwhile, people are dying because they can’t afford the follow-up scans.
And don’t even get me started on genetic testing. Who’s paying for that? Not me. Not my sister. Not my neighbor who’s working two jobs.
Meanwhile, the real problem? Poor diet, stress, no access to exercise. We’re treating symptoms with expensive lab tests while ignoring the root cause.
Also, why are all the studies funded by pharma? Coincidence? I think not.
And the fact that you’re calling it ‘HSS’ instead of HCM? That’s not just terminology-it’s erasure. This isn’t a sub-type, it’s the same disease. Stop fragmenting it for profit.