Benign Prostatic Hyperplasia and Its Impact on Kidney Function
 Oct, 3 2025
Oct, 3 2025
BPH Stage & Kidney Function Estimator
Enter values above and click calculate to see BPH stage and kidney function indicators
TL;DR
- BPH can cause urinary blockage that raises pressure in the bladder and ureters.
- High back‑pressure can damage the kidneys and lower the glomerular filtration rate (GFR).
- Early detection of rising creatinine or reduced GFR helps prevent permanent renal injury.
- Medication, lifestyle changes, and timely surgery can relieve the blockage and protect kidney health.
- Watch for symptoms like night‑time urination, weak stream, swelling in ankles, or unexplained fatigue.
Benign Prostatic Hyperplasia can cause urinary blockage that raises pressure in the bladder and ureters.
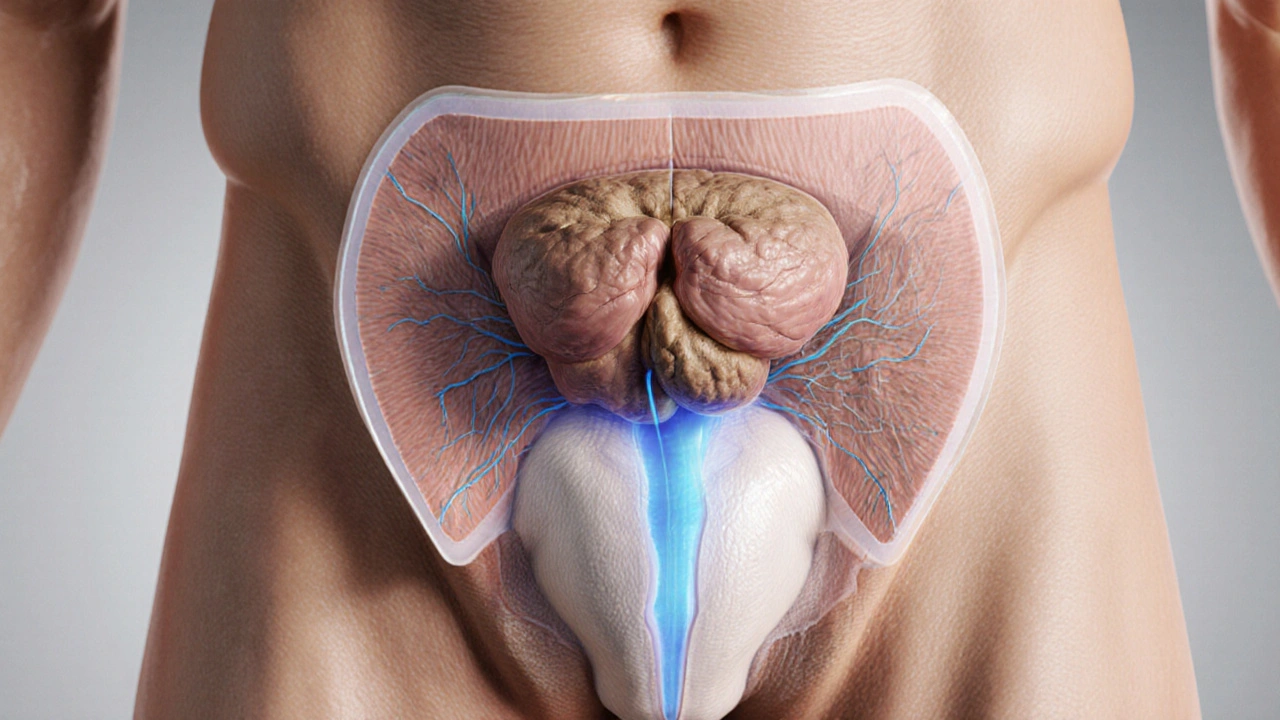
When a man over the age of 50 starts noticing frequent trips to the bathroom, a weak stream, or a feeling that the bladder never fully empties, the first suspect is often Benign Prostatic Hyperplasia is a non‑cancerous enlargement of the prostate gland that commonly causes urinary symptoms in men. While the prostate sits just below the bladder, its growth can narrow the urethra, the tube that carries urine out of the body. Over time, this narrowing creates a cascade that can reach all the way to the kidneys.
What the prostate does and why it grows
The prostate gland is a walnut‑sized organ that surrounds the urethra. Its main job is to produce fluid that nourishes sperm. Around middle age, hormonal shifts trigger the gland’s cells to multiply, leading to prostate enlargement. This process is slow, often painless, and unrelated to cancer, which is why it’s called "benign".
How urine normally flows
In a healthy system, urine travels from the kidneys through the urinary tract, passes the bladder, and exits via the urethra. The kidneys filter roughly 180liters of blood daily, turning waste into urine. The pressure inside the collecting system stays low because the bladder empties efficiently.
When the prostate swells, it can partially block the urethra. This blockage forces the bladder to work harder, creating "urinary retention" - a condition where urine remains in the bladder after voiding.
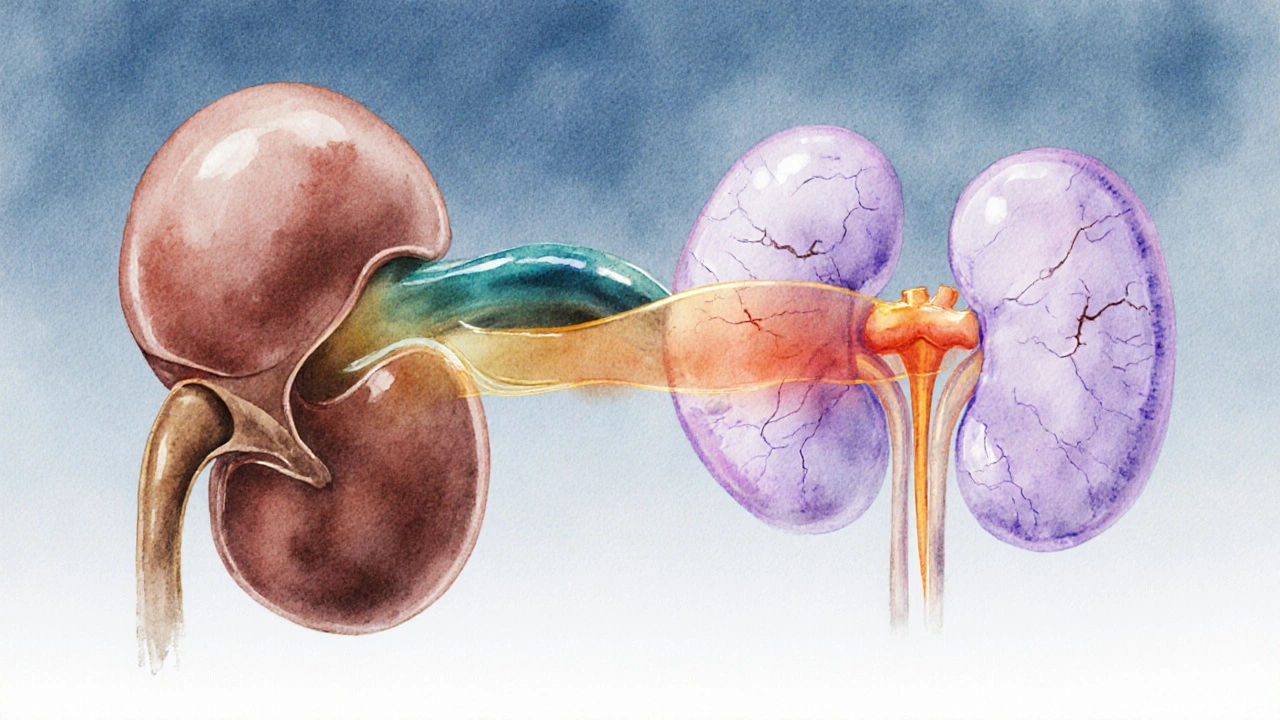
From bladder pressure to kidney injury
Persistent urinary retention pushes urine back up the ureters, the thin tubes that connect the kidneys to the bladder. The back‑flow, known as "vesicoureteral reflux," raises hydrostatic pressure around the renal pelvis. Over months or years, this pressure can:
- Reduce the glomerular filtration rate (GFR), a key measure of how well the kidneys are filtering blood.
- Cause microscopic damage to the nephrons, the functional units of the kidney.
- Elevate blood creatinine levels, a lab marker doctors use to spot early renal impairment.
In severe cases, the back‑pressure can lead to hydronephrosis - swelling of the kidney itself - which is visible on an ultrasound and often requires urgent intervention.
Warning signs that your kidneys are feeling the strain
Because kidney damage is silent until it’s advanced, you need to watch for indirect clues:
- Increased frequency of nighttime urination (nocturia) beyond normal aging.
- Swelling in the ankles, feet, or hands, indicating fluid retention.
- Unexplained fatigue or loss of appetite - early symptoms of reduced kidney clearance.
- Blood tests showing a rising serum creatinine or a drop in estimated GFR.
If any of these appear alongside classic BPH symptoms, it’s time to ask your GP for a renal panel and possibly a kidney ultrasound.
Medical tools for spotting the problem
| Stage of BPH | Typical Urinary Flow (mL/s) | Serum Creatinine (µmol/L) | Estimated GFR (mL/min/1.73m²) |
|---|---|---|---|
| Mild (IPSS 0‑7) | >15 | 70‑90 | >90 |
| Moderate (IPSS 8‑19) | 10‑15 | 90‑110 | 60‑89 |
| Severe (IPSS ≥20) | <10 | >110 | <60 |
IPSS stands for International Prostate Symptom Score, a questionnaire doctors use to gauge how much BPH is bothering you. The table shows that as the score climbs, both urine flow drops and kidney markers worsen.
How to protect your kidneys while managing BPH
Several strategies tackle the problem from both ends - relieving the blockage and guarding the kidneys.
- Medication: Alpha‑blockers (e.g., tamsulosin) relax the smooth muscle around the urethra, improving flow instantly. 5‑alpha‑reductase inhibitors (e.g., finasteride) shrink the gland over months, reducing long‑term pressure.
- Fluid timing: Spread fluid intake throughout the day, limit large volumes after dinner, and avoid caffeine or alcohol in the evening.
- Pelvic floor exercises: Strengthening the muscles that control urination can help empty the bladder more completely.
- Regular monitoring: Quarterly blood tests for creatinine and an annual ultrasound if you have moderate‑to‑severe symptoms.
- Surgical options: When medication fails, procedures like transurethral resection of the prostate (TURP) or laser vaporisation create a wider passage for urine, instantly lowering back‑pressure.
Lifestyle tweaks that make a difference
- Maintain a healthy weight - obesity increases abdominal pressure on the bladder.
- Eat a diet rich in fruits, vegetables, and whole grains; low‑salt meals ease the kidneys' workload.
- Stay active - walking or swimming improves circulation and helps regulate bladder function.
- Avoid smoking - nicotine can worsen both prostate growth and renal blood flow.
When to seek professional help
If you notice any combination of the following, book an appointment promptly:
- Persistent weak stream plus serum creatinine rising above 110µmol/L.
- Visible swelling in the lower limbs or persistent fatigue.
- Episodes of painful urination, blood in the urine, or a sudden inability to pee.
These signs may indicate that the urinary blockage is already harming the kidneys and that more aggressive treatment is needed.
Frequently Asked Questions
Can BPH cause permanent kidney damage?
Yes, if urinary obstruction is left untreated for months or years, the back‑pressure can scar nephrons and lower GFR permanently. Early treatment usually prevents irreversible loss.
How is kidney function measured in BPH patients?
Doctors look at serum creatinine, calculate estimated GFR using the CKD‑EPI formula, and may order a renal ultrasound to check for hydronephrosis.
Are there natural ways to shrink an enlarged prostate?
Some studies suggest that saw‑palmetto, pumpkin seed oil, and a high‑beta‑sitosterol diet may modestly improve symptoms, but they don’t replace proven medications for most men.
What’s the difference between TURP and laser therapy?
Both remove prostate tissue to widen the urethra. TURP uses a wire loop and has a longer hospital stay, while modern laser techniques (e.g., HoLEP) offer less bleeding and quicker recovery.
Should I get a kidney scan if I have mild BPH?
Not usually. Routine blood tests and monitoring of urinary symptoms are enough for mild cases. Imaging is reserved for moderate‑to‑severe BPH or when kidney function drops.
John Power
October 4, 2025 AT 23:13Had a buddy go through this last year - didn’t realize how serious it could get until his creatinine spiked. He was ignoring the nighttime pees for months, thought it was just "getting older." Turned out his kidneys were already stressed. Got the alpha-blocker, changed his fluid timing, and now he’s back to sleeping through the night. Don’t wait like he did.
Richard Elias
October 6, 2025 AT 17:45bro if ur prostate is big u just need to drink less water at night dumbass. why are people so lazy these days? just cut the beer and go to bed early. no surgery needed. #simplesolution
Scott McKenzie
October 7, 2025 AT 14:17Big thanks for this breakdown 🙏 I’m 58 and started noticing the weak stream last year - got my GFR checked and it was 78. Doc put me on tamsulosin and told me to track my fluid intake. It’s been 6 months and my numbers are back to 92. Early detection really saves your kidneys. Don’t ignore the signs - your future self will thank you.
Jeremy Mattocks
October 7, 2025 AT 16:26Let me tell you, this isn’t just about peeing - it’s about your whole body’s ability to detox. The kidneys are like your internal sewage plant, and when the bladder’s backed up, it’s like clogging the main line. Every time you hold it in because you’re too tired to get up at 2 a.m., you’re slowly suffocating your nephrons. It’s not dramatic, it’s biological. And once those filters get scarred, they don’t come back. That’s why I always tell my patients: if you’re waking up more than once a night, it’s not aging, it’s a warning sign. Get the ultrasound. Get the bloodwork. Don’t gamble with your kidneys - they’re the only ones you’ve got.
Paul Baker
October 7, 2025 AT 21:01my uncle had this and he just started doing kegels and now he fine 😎 no meds no surgery just pelvic floor stuff. why do docs always wanna cut stuff?
Zack Harmon
October 8, 2025 AT 15:13THIS IS WHY MEN DIE EARLY. YOU LET YOUR PROSTATE KILL YOUR KIDNEYS BECAUSE YOU’RE TOO EMBARRASSED TO GO TO THE DOCTOR. I SAW A GUY ONCE WHO WAITED 3 YEARS AND ENDED UP ON DIALYSIS. HE SAID HE THOUGHT IT WAS "JUST A PART OF AGING." NO. IT’S A SLOW MURDER. STOP BEING A WIMP.
Jeremy S.
October 9, 2025 AT 09:19Good post. Got my PSA and GFR checked last year after reading this. All clear. Still drink less coffee before bed.
Jill Ann Hays
October 10, 2025 AT 19:18It is not merely a mechanical obstruction but a systemic disruption of the homeostatic equilibrium governing renal perfusion and urinary dynamics. The pathophysiological cascade initiated by prostatic hypertrophy induces a retrograde pressure gradient which compromises glomerular integrity over time. One must therefore consider this not as a benign condition but as a chronic insidious assault on the nephron.
Mike Rothschild
October 12, 2025 AT 09:05My dad had this. He didn’t want to talk about it. Took him 5 years to get checked. By then his GFR was at 48. He’s on meds now and doing okay but he lost 20% of kidney function. Don’t be like him. Talk to your doctor. Even if it feels awkward. Your kidneys don’t care how embarrassed you are.
Ron Prince
October 14, 2025 AT 04:33why do these articles always target american men? we got the best healthcare in the world. if your prostate is bugging you go to the doc. its not rocket science. stop making it a big deal. europeans are weak. they dont even know what a real man is.
Sarah McCabe
October 15, 2025 AT 07:25My mate in Dublin had this - he thought it was just his bladder being lazy. Got the scan, turned out his kidneys were swollen like balloons. Now he’s got a stent and drinks way more water. Weird how your body screams and you just turn up the TV, right? 😅
King Splinter
October 16, 2025 AT 02:17So let me get this straight - you’re saying that if I pee slower than a snail, my kidneys are gonna implode? I mean, I’ve been peeing like this since I was 40. I’m 62 now. Still alive. Still drinking. Still not dead. Maybe the whole thing is just fearmongering by the urology industrial complex? Just saying.
Kristy Sanchez
October 16, 2025 AT 05:27Oh wow. So my fatigue and swollen ankles are because I didn’t want to admit I have a big prostate? How poetic. My body is literally crying for attention and I’m too busy scrolling TikTok to notice. Great. Now I feel like a villain in my own life story. Thanks for the guilt trip, doctor.
Michael Friend
October 16, 2025 AT 18:23This is why men are dying in silence. No one talks about this. No one. And when they do, it’s wrapped in medical jargon. I’ve seen three guys in my gym - all 55+, all ignoring it. One died of sepsis from a UTI caused by retention. The other two? Still pretending it’s "normal". We’re not fixing this. We’re just burying it.
Jerrod Davis
October 18, 2025 AT 01:43It is imperative to underscore the necessity of longitudinal monitoring of serum creatinine and estimated glomerular filtration rate in men presenting with lower urinary tract symptoms. The absence of overt pain does not preclude the presence of significant renal parenchymal compromise. Clinical vigilance remains paramount.
Dominic Fuchs
October 18, 2025 AT 20:26My grandad had this back in '87. Doctor told him to drink less tea. He did. Lived to 94. Maybe the real problem isn't the prostate - it's the fact we treat everything like a crisis now. Chill out. Your body's been doing this for centuries.
Asbury (Ash) Taylor
October 19, 2025 AT 06:40You’re not alone. I’ve coached dozens of guys through this. It’s not weakness to get help - it’s wisdom. Start with the lifestyle stuff: cut caffeine after noon, try pelvic floor exercises, keep a bladder diary. Most don’t need surgery. But they do need to pay attention. You’ve got this.
Kenneth Lewis
October 20, 2025 AT 21:35so i had a weird dream last night where my prostate was a tiny dictator and my kidneys were hostages. woke up and checked my pee flow. kinda weak. maybe i should go to the doc? 🤔
Jim Daly
October 20, 2025 AT 22:09Wait so if my prostate is big I’m gonna need surgery? What if I just hold it in longer? Build up my bladder muscles? I mean I’ve been doing that since college. I’m basically a pro at this. I bet I could train my body to ignore it.